About COM-Unity Alumni
Alumni Heading link
The 8 COM-Unities were named after the below famous UI College of Medicine Alumni and former faculty.
-
Isabella Garnett, MD (1872-1948)

On August 22, 1872, Isabella Garnett was born into the earliest African-American family to arrive in the Evanston, Illinois area. Her parents were founders of the first black Baptist church organized in Evanston. After taking business courses at a Minneapolis college, Garnett returned to the Chicago area and matriculated at the Nurse Training School of Provident Hospital, the country’s first black-owned hospital. She worked as a school nurse for two years before enrolling in a premedical program at Harvey Medical College. Garnett then enrolled at Chicago’s College of Physicians and Surgeons (known today as UIC’s Medical college) and obtained her medical degree in 1901. The courageous Garnett was one of the earliest African American women physicians in Illinois. Garnett practiced privately until 1914, when she and her husband opened the Evanston Sanitarium on the upper floors of their home.
Achievements
- 1914: Founded the Evanston Sanitarium, the first African American medical center north of the Chicago Loop
- 1939: Became superintendent of the Community Hospital of Evanston, formerly the Butler Memorial Hospital
- 1948: In the year of her passing, a day of honor was dedicated to Dr. Garnett as part of the National Negro Health Week. The US Public Health Service instituted this week in 1915, in response to data from Booker T. Washington, founder of the Tuskegee Institute The creation of National Negro Health Week resulted in the formation of the National Negro Health Movement, which formed to improve the status of Black Americans’ health year-round
Full Bio
On August 22, 1872, Isabella Garnet was born into the earliest African-American family to arrive in the Evanston area. Her parents, Daniel Garnett and Hannah McDuffin had moved into Evanston in 1864, and eventually, their family grew to include seven children. Mr. Garnett was a shoemaker and worked in his own store and several other establishments. Daniel and Hannah were founders of the Second Baptist Church (Robinson), which records this history about the founders on its website:
Second Baptist Church is the first black Baptist church organized in Evanston, Illinois. It was established on November 17, 1882, with twenty charter members in a room over the post office, which was located east of the alley on Davis Street between Chicago and Orrington Avenues. This group of former slaves consisted of ten members of the predominantly white First Baptist Church (Nathan and Ellen Branch, Daniel and Mary Garnett, George and Maria Robinson, Andrew and Susan Scott, Richard Day and William Enders) and ten other Village residents. Many were well-respected members of the community, and several owned their own businesses. The organizing pastor was the Reverend S. T. Clanton, a student at the Baptist Union Theological Seminary in Morgan Park, Illinois. (Second Baptist Church)
Leonard describes the post-Civil War cultural climate of Evanston in “Paternalism And The Rise of A Black Community in Evanston, Illinois: 1870-1930”: “At least two characteristics of Evanston during the first decades after the Civil War made the city attractive to migrating blacks…Evanston accorded blacks a degree of hospitality that was unusual…” (quoted in Robinson). Although Evanston was relatively better than most Northern cities in the Civil War and Reconstruction periods, it is important to set the broader context of the hardships into which Dr. Garnett was born. The severe racial bias in the North has been surveyed on the “Slavery in the North” histories by Harper:
When the Civil War ended, 19 of 24 Northern states did not allow blacks to vote. Nowhere did they serve on juries before 1860. They could not give testimony in 10 states, and were prevented from assembling in two. Several western states had prohibited free blacks from entering the state. Blacks who entered Illinois and stayed more than 10 days were guilty of “high misdemeanor.” Even those that didn’t exclude blacks debated doing so and had discriminatory ordinances on the local level. (Harper)
Garnett attended high school in Evanston and went on to take business courses at a Minneapolis college. After coming back to the Chicago area, she matriculated at the Provident Hospital Nurse Training School in 1895 (Evanston’s History Center). Provident Hospital was the country’s first black-owned hospital. Garnett worked as a school nurse for 2 years in this period of early training. Following Nursing School, Garnett entered the Harvey Medical College between 1897-99 and earned a premedical certificate (Wikipedia citing Dreger). After attaining her certificate, Garnett enrolled at Chicago’s College of Physicians and Surgeons (known today as UIC’s Medical college) and obtained her medical degree in 1901 (Evanston Women’s History Project). The courageous Garnett was one of the earliest African American women physicians in Illinois (Illinois State Museum web page).
After interning on the South Side of Chicago, Dr. Garnett moved back to Evanston in 1904, and 3 years later she married Dr. Arthur Butler in 1907 (Evanston Women’s History Project). Dr. Arthur Butler was one of very few African American medical school graduates of Northwestern University (Hubbard).
Garnett continued to practice privately until 1914 when she and her husband opened the Evanston Sanitarium. This training school and care facility was established on the upper floor of the couple’s house in Evanston (Evanston Women’s History Project).
In JNMA’s 1953 running commentary, “The Integration Battle Front,” notes some of the collaborative forces that moved to found this health clinic in order to serve the massively underserved black population in the area: “the two physicians were aided in their undertaking by many of the most eminent physicians and surgeons of Evanston the North Shore” (The New Community Hospital…). The commentary goes on to offer readers a fuller view of the story, however, citing the historical racially biased practices in the Evanston and Chicago area hospitals, which had longstanding patterns of refusing to offer services to African Americans. At the time, only one of 4 hospitals in the Chicago area accepted African American patients and employed African American physicians. Hubbard comments: “The inherent cruelty involved in dealing with so vital a matter as health along racial lines has received editorial comment in this Journal” (The New Community Hospital…).
The Garnett’s Sanitarium, which addressed the community’s urgent needs was the first African American medical center established north of the Chicago Loop. Garnett’s husband served as the Sanitarium’s only surgeon and general practitioner, working in anesthesia and obstetrics until he died in 1924. After Dr. Butler’s death, Dr. Garnett managed the Sanitarium on her own, funding it with income from her own practice. She renamed the hospital as the “Butler Memorial Hospital” in honor of her beloved husband (Evanston Women’s History Project).
The Butler Memorial Hospital saw a huge increase of patients with the occurrence of the Great Migration, the period 1910-1925 when African Americans moved from the Southern states to the Northern States in search of a better living and relief from the Jim Crow culture. During this period, Garnett’s tiny 3- room 2-story facility was a “lifeline” of medical treatment for thousands of African American residents for the over 50 years it functioned. Many of those who benefited from the Garnett-Butler achievement were living witnesses to the dire need their hospital supplied. Tribute reporter, Tracy Dell’Angela interviewed 76-year old Laverne Strickland in 1996 about the hospital where she was born and the de facto segregation of the time. Strickland said, “It was a known fact that you did not try to go to the white hospitals. Unless you were dying, you were not welcome” (Dell’Angela).
In 1930, Garnett married Baptist minister, James Talley. In the same year, the Butler Memorial Hospital merged with the Booker T. Washington Association of Evanston, relocated, and took on a new name, The Community Hospital of Evanston. The new hospital started in the house of Dr. Rudolph Penn as an 18-bed facility. From 1939 to 1945, Isabella Garnett served officially as the organization’s superintendent (Evanston Women’s History Project).
Isabella Garnett retired in 1946 after a magnificent career of service and building. In 1948, she passed away from cardiac complications at age 76 in the hospital she built.
Earlier in 1948, the year of Dr. Garnett’s passing, a day of honor was dedicated to her as part of the National Negro Health Week. Tiffany Walker, Archives Technician at the National Archives at College Park, Maryland posted the following entry describing this week and its meaning in the forward movement toward caring for African American citizens:
“National Negro Health Week” began in 1915, in response to disturbing findings by the Tuskegee Institute that highlighted the poor health status of African Americans in the early part of the 20th Century. At a session of the Tuskegee Negro Conference in 1914, founder of the Tuskegee Institute, Booker T. Washington brought forth data, which showed the economic costs of the poor health status of the black population in the United States.
The U. S. Public Health Service then instituted “National Negro Health Week” in response to these findings, in order to improve the health status of the black population by educating members of the community, providing greater access to healthcare, and encouraging an increased number of black professionals in the field of public health. National Negro Health Week was observed during the first week of April, and focused on educating black communities throughout America on methods of acquiring health care and informing students on proper health practices.
The creation of National Negro Health Week resulted in the formation of the National Negro Health Movement, which formed to improve the status of black health in America year round. Organizations that participated in this movement included the Annual Tuskegee Negro Conference, the National Medical Association, the National Negro Business League, and the National Negro Insurance Association. The movement, in collaboration with the U. S. Public Health Service, published the “National Negro Health News” quarterly. The publication focused on planning for annual National Negro Health Week activities, as well as reporting on new data and reports related to the status of black health. (Walker)
We note that our Dr. Isabella Garnet Butler was in the vanguard of this movement.
The Evanston Community Hospital Dr. Garnett started was expanded to a new facility in October 1952. The JNMA reported in 1953 on the modern new facility, which Garnett had envisioned and brought into being:
“The new hospital has fifty-four beds in two bed-rooms, a nursery with twelve bassinets, two operating rooms and two delivery rooms. It is built on one floor and cost $940,000. $15,000 is still needed for equipment and $40,000 more to convert the old hospital building into quarters for nurses. $394,000 was contributed under one Federal grant approved by the U. S. Public Health Service in November 1950. Additional public aid in the sum of $56,000 has been announced…” (The New Community Hospital…)
In 1975, a park near the hospital was dedicated as the “Isabella G. Butler Park” (Evanston Women’s History Project).
Works Cited
- Illinois State Museum, Research and Collections website. “Dr. Isabella (Garnett) Butler’s medical bag and instruments.” Accessed May 2020 at: http://story.illinoisstatemuseum.org/content/dr-isabella-garnett-butler%E2%80%99s-medical-bag-and-instruments
- The New Community Hospital of Evanston, Illinois. J Natl Med Assoc. 1953;45(1):74-75. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2617163/pdf/jnma00611-0078.pdf
- Harper, D. (2003). Slavery in the North (website). Accessed May 2020 at: http://slavenorth.com/exclusion.htm
- Evanston Women’s History Project. “Isabella Maude Garnett.“ The Evanston History Center, Evanston, IL. Accessed May 2020 at: https://evanstonwomen.org/woman/isabella-maude-garnett/
- Perkins, M. B. (2013). Evanston: A Tour Through the City’s History. United States: Evanston History Center. (Preview in Google Books)
- Records of the Evanston Sanitarium, the Community Hospital of Evanston and the Community Hospital Women’s Auxiliary. Biograph or history web page. Accessed May 2020 at: https://connect.historyit.com/PublicSites/browse/671?account=evanstonhistorycenter
- Robinson, M. E. (1997). A place we can call our home: The emerging Black community circa, 1850-1930. Evanston, Ill: M.E. Robinson.
- Second Baptist Church web page. “A Summary History of Second Baptist Church.” Compiled by Rhonda K. Craven, Church Historian. Access May 2020 at: https://www.secondbaptistevanston.org/history
- Tracy Dell’Angela (Novemeber 17, 1996). “Laverne Strickland: Black Hospitals Held Out Hope At A time When White Hospitals Shut The Doors.” Chicago Tribune. Retrieved May 20, 2020. Chicago Tributne.com. Accessed May 2020 at: https://www.chicagotribune.com/news/ct-xpm-1996-11-17-9701150137-story.html
- Walker, T. “National Negro Health Week: 1915 to 1951.” Posted March 29, 2016 in African-American Women, Civil Rights. Accessed May 2020 at: https://rediscovering-black-history.blogs.archives.gov/2016/03/29/national-negro-health-week-1915-to-1951/
- Wikipedia contributors. (2020, May 8). Isabella Garnett. In Wikipedia, The Free Encyclopedia. Accessed May 2020 at: https://en.wikipedia.org/w/index.php?title=Isabella_Garnett&oldid=955477089 . Wikipedia citing Dreger. Dreger, Marianne; Wishart, Patricia C. (1990). “Garnett Butler Talley, Isabella Maude”. In Schulz; Hast (eds.). Women Building Chicago, 1790-1990. Indiana University Press. pp. 303–306.
-
Rachelle Yarros, MD (1869-1946)

Rachelle Slobindsky Yarros immigrated to the United States from Russia as a teenager. As a member of a revolutionist political party, she always feared being arrested by the Czar’s police. In the US, she worked in a sweatshop before enrolling as the first woman to enter in the College of Physicians and Surgeons in Boston. She finished medical school at the Woman’s Medical College of Pennsylvania, then moved to Chicago to complete her residency at Michael Reese Hospital. Yarros spent the next 40 years on faculty at University of Illinois in women’s health. She was a resident of Hull House, the famous social settlement that nurtured leaders in social welfare. She was a leader in the birth control movement, and she challenged the attitudes, policies, and practices that denied women access to birth control information and devices. She established the first birth control clinics throughout the city of Chicago; she was a dedicated campaigner for sex education for women.
Achievements
- In 1914, Dr. Yarros helped found the American Social Hygiene Association, which today is known as the American Sexual Health Association. She also founded and directed the Illinois Birth Control League.
- In 1923, Dr. Yarros opened the second birth control clinic in the United States and by 1930, Chicago had 8 birth control clinics throughout the city, more than any other American city.
Full bio
Rachelle Slobodinsky Yarros was born May 18, 1869, near Kiev, in Berdechev, Russia. Her parents, Joachim and Bernice Slobodinsky were prosperous, and Rachelle was educated in Russian schools. As a teenager, she joined a revolutionist political group, against her family’s wishes. Eventually, she realized that she might be arrested by the Czar’s police and accepted her families’ money to emigrate to the United States around her 17th or 18th year (Perry). After she arrived in the U.S., Slobodinsky made a living sewing in the sweatshops in New York and New Jersey, where she lived and worked among the poor (Lasch). At the New Jersey sweatshop, Slobodinsky organized a strike (Perry), and although the strike failed, Slobodinsky would go on to organize many other successful group actions for social justice in her life.
In 1890, emigre friends persuaded Slobodinsky to enroll in medical school and funded her efforts. Slobodinsky became the first woman admitted to the College of Physicians and Surgeons in Boston. At this time, she began work in nursing care at the Tewksbury State Institution. After a year of medical school in Boston, Slobodinsky moved to Philadelphia, finishing her medical degree at the Woman’s Medical College of Pennsylvania in 1893. Subsequently, she interned at the New England Hospital for Women and Children, and eventually went on to postdoctoral work at the New York Infirmary for Infants and Children (Perry).
Christopher Lasch describes Slobodinsky’s relationship with her husband Victor Yarros, “Moving to Boston, she met a fellow countryman, the journalist and philosophical anarchist Victor S. Yarros, to whom she was married on July 18, 1894. They had no children of their own but eventually adopted a daughter, Elise Donaldson” (Lasch). Lasch notes Yarros’ support for his wife’s ongoing education and career. When the couple settled in Chicago and she began her obstetrical and gynecological practice in 1895, Victor Yarros pursued his career in journalism and law (Lasch).
Rachel Yarros undertook residency training at Michael Reese Hospital in Chicago. After completing her residency and starting her practice on Chicago’s West Side, Yarros worked as an unsalaried teacher in clinical Obstetrics at the University of Illinois at Chicago. Perry describes Yarros’ philosophy of teaching and practice:
She thought students should have hands-on instruction by assisting her with home deliveries at the dispensary, and within the year she had convinced the dean to permit the program. Called by students the ‘Department of Obstetrics in the Ghetto,’ this medical training enabled babies to be delivered under the safest and most sanitary conditions. The program ran for twelve years. (Perry)
Yarros’ work at UI in obstetrics, home birth, sexuality, and birth control as a clinician and educator was groundbreaking and remarkably responsive to community needs. In modern times, it is difficult to imagine conditions in Chicago a century ago, but when Yarros began working, there was no organized service system for women in healthcare. At the time, Yarros gained sponsorship for her clinic, because the school had no teaching facilities for obstetrics (Ray).
Yarros became an associate professor at UI in 1902 and remained at UI for most of her career. In 1926, UI created a special professorship to honor her work in Social Hygiene and she held the appointment until 1939 (Lasch).
Between 1907-1927, Yarros was a resident at Hull House in Chicago. Hull House was an extraordinary environment for nurturing many leaders in social welfare and healthcare transformation. Yarros and her husband, Victor, both identified with the social settlement movements inspired by Jane Addams, Margaret Sanger, and other reformers. Yarros’ longtime collaborator, Alice Hamilton, developed a relationship with Yarros at Hull House, and eventually Hamilton went on to become first woman faculty member at Harvard’s School of Medicine (Haslett). The settlement and social hygiene movements of this era addressed the needs of the urban poor and immigrants struggling with the social breakdown brought on by industrialization and the hardships of carving out a new life after fleeing poverty and oppression in their native lands. The struggle to overcome these collective survival issues led to the establishment of the famous settlement house in Chicago known as Hull House, which according to Jane Addams’ was purposed “to provide a center for a higher civic and social life; to institute and maintain educational and philanthropic enterprises and to investigate and improve the conditions in the industrial districts of Chicago” (Addams).
In Maurice Hamington’s philosophical work, “Embodied care: Jane Addams, Maurice Merleau-Ponty, and Feminist Ethics,” Hamington describes the social dynamism of “proactive embodied care” espoused by Addams as leading to enduring friendships and “a woman-centered activist environment that brought together some of the great minds of the time”:
There were probably few venues where women of such achievement worked, lived, and socialized together. Eleanor Stebner suggests that friendship was an important aspect of Hull-House’s success: “The friendships made and fostered at Hull House enlarged the personal worlds of each woman. They helped each woman identify her unique vocation, and served as a basis for her social and political involvement.”86 …The personal relationships among Hull House residents fueled their activism and modeled the spirit of connection they sought with the neighborhood at large. One of their efforts to connect the community was a series of social clubs whose activities centered on the arts, education, politics, or many times simply socialization. (Hamington)
In 1914, Yarros helped found the American Social Hygiene Association (ASHA), which is known today as the American Sexual Health Association. Yarros’ motivation for this effort appears to stem from early treatment she had done as a volunteer in a Massachusetts asylum with syphilitic patients (Perry). The mission of the ASHA was “to stop the venereal disease epidemic by educating the public about sexually transmitted infections, working to break down the social stigma attached to VD, and encouraging high moral standards” (American Social Hygiene Association History and a Forecast website).
Yarros was also the first vice president of the Illinois Social Hygiene League, which was founded originally as The Red League. The League’s mission was the same as the mission of the ASHA, to fight the spread of venereal disease through sexual education (Institute for Sex Education Records). Both the ASHA and the ISHL worked to stop the spread of sexually transmitted diseases that would eventually afflict the most vulnerable, including soldiers with little education in hygienic practices who traveled abroad and returned throughout World War I.
After World War I started, Yarros convinced the Chicago Women’s Club, where she was a member, to establish a birth control committee, which eventually evolved into the Illinois Birth Control League (IBCL). Yarros directed the IBCL for many years in her efforts to empower women’s reproductive self-determination (Perry). In 1923, when Yarros opened the nation’s second birth control clinic close to Hull House, she inspired the creation of similar clinics across the city. Haslett writes extensively on the achievements of Yarros and Hamilton, documenting the widening circle of impact emanating from the provision of birth control services:
As their association with the birth control movement evolved, they challenged the attitudes, policies, and practices that denied women access to birth control information and devices. They also created programs to provide concrete services, such as medical centers that offered a broad range of health care and information, including contraception, and supportive services for day nurseries, particularly for working mothers and their children. (Haslett)
At the core of Yarros’ achievements, was the essential need to establish birth control clinics to enable the limitation of family size, reducing infant mortality and the great hardships large families often carried for the immigrants and the poor. Yarros and her physician-scholar colleagues made distinct contributions to this movement from their place in the academy, working to promote the kinds of research needed to convince physicians that birth control and its research mattered. In 1931, Yarros wrote:
“One of the most valuable means of removing such apathy as exists [among physicians] is the systematic reporting of findings based on experience with the large numbers of cases, such as are treated by the birth control clinics conducted under proper supervision. Exchanging this information and making it available for the use of physicians generally will help to determine the best methods available and greatly increase the appreciation of birth control as a means of promoting health and welfare.” (Haslett)
Yarros was a dedicated campaigner for sex education for women. She hoped abortions would not be necessary through the development of effective methods of sexual education for women (Haslett). Yarros furthered public education through civic action societies and widespread programs. Perry described Yarros’ perspective and courage in reaching out to the suffering women of her time:
Yarros fully supported disseminating contraceptive information to working-class women to ensure a healthier way of life. She had witnessed the effects on immigrant women who had undergone abortions, often self-induced. Some women had suffered serious problems requiring surgery, others had chronic inflammations. Inspired by hearing Margaret Sanger speak and aided by the Illinois Birth Control League, she opened the second birth control clinic in the United States in 1923. She defied opposition from the Roman Catholic clergy and health officials by opening a medical center and clinic that distributed contraceptive literature in the business district in 1924. Encouraged by the strong response she received, Yarros opened additional centers in ethnic and minority neighborhoods. By 1930 Chicago had eight birth control clinics, more than any other American city. (Perry)
Throughout her entire life, Yarros remained engaged in movements to better healthcare in society. In 1932, Yarros established the first pre-marital counseling clinic in the Midwest. She was opposed to the eugenics movement of time and a strong advocate of reproductive freedom. Haslett lauds her “celebration of diversity” and the use of her understanding of culture in the treatment women (Haslett). She describes Yarrow tremendous insight into service delivery as well: “Yarros understood the need for seamless services, beginning with sex education and premarital and marital counseling and ending with birth control clinics accessible to working mothers, thus providing supportive services at each stage of a woman’s sexual life and reproductive journey” (Haslett).
Dr. Yarros’ imprint as a physician, researcher, scholar, community organizer, healthcare delivery innovator, friend and inspired teacher is emblazoned on the cradle of the women’s healthcare in the modern age.
Works Cited
- Addams, Jane. Twenty Years at Hull-House: with Autobiographical Notes. Macmillan, 1922.
- “American Social Hygiene Association History and a Forecast.” Social Welfare History Project, 6 Mar. 2018. Accessed May 2020 at: https://socialwelfare.library.vcu.edu/programs/health-nutrition/american-social-hygiene-association-history-and-a-forecast/
- Hamington, M. (2004). Embodied care : Jane Addams, Maurice Merleau-Ponty, and Feminist Ethics. Accessed May 2020 at: https://search-proquest-com.proxy.cc.uic.edu/docview/2131132765/F2E902B5A93B4228PQ/1?accountid=14552
- Haslett, D. C. (1997). Hull House and the Birth Control Movement: An Untold Story. Affilia, 12(3), 261–277. https://doi.org/10.1177/088610999701200302
- Perry, M. (2000, February). Yarros, Rachelle (1869-1946), physician and reformer. American National Biography. Accessed May 2020 at: https://www.anb.org/view/10.1093/anb/9780198606697.001.0001/anb-9780198606697-e-1201753
- Ray, J. M. (1992). Women and men in American medicine, 1849-1925: autobiographies as evidence (Doctoral dissertation, University of Texas at Austin).
- Lasch, C. (1971). “Yarros, Rachelle Slobodinsky.” In E. T. James, J. James, & P. Boyer (Eds.), Notable American Women, 1607-1950, Volume III: P-Z (p. 690). Cambridge, MA: Harvard University Press. Retrieved from Women and Social Movements in the United States,1600-2000 database. Accessed May 2020 at: https://search-alexanderstreet-com.proxy.cc.uic.edu/view/work/bibliographic_entity%7Cbibliographic_details%7C2515557?dorpID=1000169008#page/690/mode/1/chapter/bibliographic_entity%7Cdocument%7C2516114
-
Dr. Olga Jonasson

Dr. Olga Jonasson was born in Peoria, Illinois to parents of Swedish immigrants. As a youngster, Jonasson was influenced by witnessing the work of her mother, a nurse, and her father, a pastor, in caring for the sick. She completed her bachelor’s degree in 1956 at Northwestern, and her medical degree at University of Illinois in 1958. When Jonasson decided to apply for a surgical residency, there were very few women practicing in this area. She completed residency in 1964, followed by three fellowships, one of which was at Massachusetts General Hospital in transplantation immunobiology. She joined the faculty of University of Illinois in 1967, where she developed the Division of Transplantation. Throughout her career, she served as a mentor and role-model for young female surgeons. In 1993, she became the Medical Director of the Education and Surgical Services Department of the American College of Surgeons, the first female surgeon to do so.
Achievements
- 1968- Dr. Jonasson performed the first kidney transplant in Illinois
- 1976- Dr. Jonasson was named the first woman to serve on the American College of Surgery Board of Regents
- 1977- Dr. Jonasson was named the new Chief of Surgery at Cook County Hospital
- 1983- Dr. Jonasson chaired the national task force that issued a White Paper which provided broad guidelines for implementation of the newly passed National Organ Transplant Act
- 2006- The Association of Women Surgeons renamed their Distinguished Member Award the Olga Jonasson Distinguished Member Award
Full Bio
Olga Jonasson was born August 12, 1934 in Peoria, Illinois to Swedish immigrants, Olav and Swea Jonasson. When she was 12, her family migrated to Chicago, where Olav took up the pastorship of Ebenezer Lutheran Church in the Andersonville neighborhood (Husser). The church was center of faith and culture for the Swedish community (Ebenezer Lutheran Church, “Who we are”). As a youngster, Jonasson was influenced by witnessing both of her parents’ work in caring for the sick. She went with her father on visits to shut-in parishioners and she accompanied her mother, a nurse, to the hospital. Jonasson watched and recounted what she had learned:
My mother’s nursing career was of great interest to me as a child, and when my clergyman father made hospital visits, I came along and loved sitting in the lobby watching what was happening. My decision to become a physician seemed to be a natural evolution of these interests and I do not remember having other aspirations. The act of actually intervening in someone’s suffering was a prime motivation, and the active nature of surgery was particularly interesting and involving. (Changing Face of Medicine)
Jonasson’s early self-reliance was apparent when she stayed back in Chicago to study at Northwestern University at the age of 16, while her family moved to on to Connecticut. She attended Northwestern University from 1951 to 1954 and then entered the University of Illinois. She completed her bachelor’s degree in 1956. Jonasson finished her medical degree with honors in 1958 at the University of Illinois, and went on to complete her internship at UI’s hospital. While attending medical school, the energetic Jonasson worked at the North Shore lab where she performed analysis of blood and urine. She was also elected to the distinguished Alpha Omega Alpha medical honor society. When Jonasson decided to apply for a surgical residency, there were very few women practicing in this area. She faced many doubts among her faculty, but through great persistence was eventually able to persuade Dr. Warren Cole that her aim was not ‘preposterous’ and he accepted her into the surgical residency program at the University of Illinois Research and Education Hospital (Ennis). Thus, Dr. Jonasson began an extraordinary career as a woman in surgery and cut a groundbreaking path for those who would follow.
Jonasson graduated her residency program in 1964. Her first fellowship in immunochemistry at Walter Reed Army Institute of Research, was followed by another fellowship at the Massachusetts General Hospital of the Harvard Medical School in transplantation immunobiology, and a third fellowship in cardiovascular and thoracic surgery was completed in Chicago (Ennis).
In 1966, Dr. Jonasson became the 37th woman to receive certification from the American Board of Surgery among over 14,000 men (Batholomew). She worked as a cardiovascular surgeon at Rush Presbyterian Hospital until she resigned to accept a position at the University of Illinois Hospital in 1967 (Ennis). She developed the division of transplantation at the University of Illinois Hospital in 1968, and performed the first kidney transplant in Illinois the same year. In 1969, the National Institutes of Health funded Jonasson’s investigation of kidney tissue typing for transplant recipients. Her pioneering work resulted in the establishment of a tissue typing laboratory for 6 transplantation centers in Chicago (Husser).
Dr. Jonasson’s career was studded with many firsts as she pioneered the way for women surgeons. In 1976, Jonasson was named the first woman to serve on the American College of Surgery Board of Regents, and in 1977, she achieved another first for a woman as the new Chief of Surgery at Cook County Hospital (Ennis). When Jonasson left Cook County Hospital in 1987 to take up the mantle of Chair of Surgery at Ohio State University and became the Robert M. Zollinger Professor of Surgery, she was the first female in a coeducational school in the United States to achieve this rank. In 1993, she left Ohio State University and returned to Chicago where she became the Medical Director of the Education and Surgical Services Department of the American College of Surgeon (Husser). According to the American College of Surgeons “She was the first female surgeon to hold a high-level staff position within the College’s Executive Staff” (“Olga Jonasson, MD, FACS, 1934-2006”).
As the Director of Education and Surgical Services at the American College of Surgeons from 1993 to 2004, Jonasson was engaged in setting the field’s agenda for research and the forward movement of numerous patient safety initiatives. She was a leader in getting funding for the National Surgical Quality Improvement Program and advancing studies to investigate the working conditions of residents. These conditions impacted patient outcomes. More than $13 million dollars of research money moved under her leadership during the period of her directorship for ACS (Husser).
Much of Jonasson’s persistent regard and honor among colleagues and trainees in her field arises from the work she put into mentoring and teaching others, including medical students, residents, and faculty. Husser describes Jonasson’s profound professional generativity:
She was tireless in her deliberate actions to ensure the success of her protege´s. She was very secure in her own accomplishments, which allowed her to enjoy great personal satisfaction in the success of those fortunate enough to have worked with her. Whether it was editing manuscripts, assisting in writing grants, saving a place in line at the microphone at national meetings, her efforts were unending in enabling and encouraging younger surgeons. In honor and memory of her unwavering efforts, especially for young women surgeons, the Association of Women Surgeons has renamed their Distinguished Member Award the Olga Jonasson Distinguished Member Award. (Husser)
Jonasson was made an honorary member of the American College of Black Academic Surgeons based on her “outstanding mentorship of minority surgeons,” and she received multiple Golden Apple Awards for her “lively and rigorous student/resident teaching” reflecting her commitment to excellence (Bartholomew). Of note, was Dr. Jonasson’s dinner for trainees:
The Chief’s club, a three-decade-long monthly tradition of dinner for chief residents held in her home, was prized (and feared) for the after dinner Socratic ‘grilling’ by an invited expert. She opened her heart and her home to furnish newly emerging surgeons with the art and critical thinking needed in excellent surgical practice. (Bartholomew)
After Jonasson’s passing, many reflected on her as a teacher and mentor. Jeremy Pearce, reporting for the New York Times, spoke with Dr. Truman Anderson about Jonasson’s gifts as a teacher. Anderson, a former dean at the Illinois medical school, memorialized her “remarkable skills as a surgeon” and her facility in teaching residents and surgeons in training: “[She] proved that in teaching students setting an example is more than important — it is the only thing” (Pearce).
In addition to her mentoring work, Dr. Jonasson contributed in the challenging arena of national policy development, which was fraught with strife and contest. In 1983, the National Organ Transplant Act was passed and Jonasson was took up the role of Chairperson for the group charged with setting forward the details of the enactment and enforcement policies for the new law. Bartholomew writes:
As a policy instrument, she was the lightning rod to which wildly disparate points of view, ugly protests and bitter criticisms of the law itself were directed. She presided over her task force with dignity and always with intelligence and firmness. Olga could not be swayed by false arguments. She had an uncanny ability to identify people who were lying or were out for personal gain. After it was all over, many people took credit for the resulting American transplant system that quickly became an object of national pride, and a world-wide standard. The one individual who never claimed any kind of personal credit was Olga Jonasson. Yet, we all knew that nothing could have been accomplished without the presence of this magnificent leader. (Bartholomew)
Dr. Jonasson was honored for her service may times. In 1996, Jonasson was honored by the University Alumni Association for her long history of achievements (Husser). She was an honorary fellow of England’s Royal College of Surgeons, a Markle Scholar in Academic Medicine, and recipient of the Elizabeth Blackwell Award of the American Medical Women’s Association. She worked in her specialty area to advance standards with the Accreditation Council for Graduate Medical Education. Dr. Jonasson was on the editorial boards for the Annals of Surgery and the Journal of the American College of Surgeons as well as a frequent reviewer for the Journal of the American Medical Association and the New England Journal of Medicine. (Changing Face of Medicine).
On August 30th, 2006, Dr. Olga Jonasson died at Northwestern Memorial Hospital of T-cell lymphoma. She was 72 years old. In 2007, the American College of Surgeons established the Olga M. Jonasson Lecture in her honor.
Works Cited
- Bartholomew, A., Ascher, N., & Starzl, T. (2007). TRIBUTE: Dr. Olga Jonasson Born in Peoria, Illinois, August 12, 1934 Died in Chicago, Illinois, August 30, 2006. American Journal of Transplantation, 7(8), 1882-1883. Accessed May 2020 at: onlinelibrary.wiley.com/doi/full/10.1111/j.1600-6143.2007.01872.x
- Changing the Face of Medicine. Biography: Dr. Olga Jonasson. National Library of Medicine website. Accessed May 2020 at: https://cfmedicine.nlm.nih.gov/physicians/biography_174.html
- Ebenezer Lutheran Church: Who we are. (2020). Accessed May 2020 at: http://ebenezerchurch.org/whoweare/history/
- Ennis, L. A. (2010). Jonasson, Olga. In A. Markoe, K. Markoe, & K. T. Jackson (Eds.), The Scribner Encyclopedia of American Lives (Vol. 8, pp. 255-256). Detroit, MI: Charles Scribner’s Sons. Accessed May 2020 at: https://link-gale-com.proxy.cc.uic.edu/apps/doc/CX1347100151/GVRL?u=uic&sid=GVRL&xid=7f0372f9
- Husser, W., & Neumayer, L. (2006). Olga Jonasson, MD: surgeon, mentor, teacher, friend. Annals of Surgery, 244(6), 839. Accessed May 2020 at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1856623/
- Pearce, Jeremy. “Olga Jonasson, 72, Surgeon and a Role Model for Women, Dies.” New York Times. Accessed May 2020 at: https://www.nytimes.com/2006/09/13/obituaries/13jonasson.html
- “Olga Jonasson, MD, FACS (1934-2006).” American College of Surgeons. Accessed May 2020 at: www.facs.org/about-acs/archives/pasthighlights/jonassonhighlight
- Stone, E. (2006, Sep 12). Dr. Olga Jonasson: 1934 – 2006 ; Professor blazed trail for female surgeons; pioneer in organ transplants also hailed as phenomenal teacher at UIC. Chicago Tribune Final Edition. Accessed May 2020 at: http://proxy.cc.uic.edu/login?url=https://search-proquest-com.proxy.cc.uic.edu/docview/420461487?accountid=14552
-
Julius Richmond, MD, MS (1916-2008)

Dr. Julius Richmond’s talent for diplomacy was exceptional and matched by a genius for advancing public health. During his internship and residency at Cook County Hospital he witnessed the profound impact of poverty on child health. Figuring out how to help the most people in the most cost-effective way was to become Richmond’s lifelong mission.
His three crowning accomplishments in public health, according to pediatrician and author Judith Palfrey, were the founding of the Head Start program, the neighborhood health center movement, and the landmark public policy declaration in 1979, entitled “The Surgeon General’s Report on Health Promotion and Disease Prevention.”In 1971,Richmond was appointed to lead two departments at Harvard Medical School: the Department of Child Psychiatry and Human Development and the Department of Preventive and Social Medicine. In 1977, President Jimmy Carter appointed Richmond as the 12th Surgeon General of the United States and Assistant Secretary for Health.
Achievements
- 1979- Richmond issued “The Surgeon General’s Report on Health Promotion and Disease Prevention” report. This Healthy People Report reflects Richmond’s genius as a strategic communicator and is still the major policy document informing our national and state public health agendas to this day
- 1979- Richmond issued the “Smoking and Health” report to help advance life saving public health change through tobacco control
Full Bio
Dr. Julius Richmond’s talent for diplomacy was exceptional and matched by a genius for advancing public health. Richmond was able to move seamlessly between many diverse groups in society. He shifted frequently between academic and governmental medicine roles throughout his career and accomplished magnificent feats on behalf of the nation as a result.
Richmond was born on September 26, 1916, to a Russian-Jewish immigrant family. Richmond’s biographer, Charles Bussey, paints a portrait of Richmond’s family and early life as deeply influential of the man he would become:
“My parents,” he said, “fled Czarist rule in Russia and settled in Chicago. My early recollections are that my parents emphasized excellence and community service.” Jacob and Anna Richmond took their son to Jane Addams’s famed Hull House and exposed him to the remarkable ideas and achievements of the women there, who dedicated themselves to securing child labor laws, educational opportunities, and health services, especially for children. Women like Florence Kelly, Alice Hamilton, and Julia Lathrope provided models for institutionalizing services (infant welfare stations, children’s courts, the pioneer child guidance clinic) for the rest of the century. Richmond’s exposure to the example of Hull House occurred between the ages of six and ten, for his mother died in 1927 with a brain tumor. She and Jacob—Richmond refers to them as “social democrats and activists on behalf of others”—planted in their son’s mind the idea that he could make a difference in society. He did. (Bussey)
After his mother’s passing, young Richmond attended Allendale boarding school in the countryside, where he was the only Jewish student. Richmond recollected the period as a cultural adventure, “an experience in group living and got me out into a cultural setting different from the one in which I had been growing up. I had an opportunity to see contrasts and to get a comparative view” (Bussey).
When Richmond graduated from John Marshall High School in Chicago, he matriculated as an undergraduate at the University of Illinois Urbana-Champaign. Threads of his destiny met him there. During a demonstration in Urbana opposing the University’s housing segregation policies, Richmond met the woman he would marry, Rhee Chidekel. In this period, Richmond’s humanitarian concern for socio-economic inequity also emerged as a scholarly focus. In the tragic period of the Great Depression, the undergraduate published his first paper, “American Serfdom,” a critical look at share-cropping in the American South (Bussey).
In 1937, Richmond attended medical school at the University of Illinois in Chicago, where he graduated post haste with both a medical degree and a master’s in physiology (1939). During this intensely formative time, Richmond discovered a publication from the Committee on the Costs of Medical Care, which would prove to be life-altering. Figuring out how to help the most people in the most cost-effective way was to become Richmond’s lifelong mission (Bussey).
As a graduate student in medicine, Richmond undertook an 18-month internship at Cook County Hospital and followed it with two residencies in pediatrics. Between 1941-1942, he served as house staff at Chicago’s Municipal Contagious Disease Hospital, and he followed with a second residency at Cook County Hospital (History of Medicine). Bussey describes Richmond’s distressing experience working with the poor in his residency in the depression era before many of our modern social services—and his resilient social activism:
He found it challenging, but disconcerting. “Our experience with poverty there,” he remembers, “was simply overwhelming. We were in no way prepared for it. Humor became the defensive armor against looking at it too deeply. It was M*A*S*H*-like humor, over-done, and I thought what an unfortunate experience it was to have to behave as though you were really insensitive to it.” Herb Abrams and Marc Hollander, fellow interns/residents, describe the situation in similar terms. Hollander remembers Richmond as “a walking encyclopedia of pediatrics.” According to Hollander, who was an intern while Richmond was a resident, “Julie organized a march on City Hall to improve conditions for interns.” The result: “We started to get paid. I got $12 a month!” Hollander said. But Richmond and his fellow students were most “impressed by the impact of poverty.” They dealt only with the poverty population at Cook County. (Bussey)
With the onset of World War 2, in February 1942, Richmond volunteered for service with the Army Air Corps. There he practiced as a flight surgeon with the service’s training command until 1946.
Richmond returned to Chicago in 1946 to complete the residency at Cook County, and he was subsequently recruited to become a Professor of Pediatrics at the University of Illinois Medical School. His biographer outlined several features of Richmond’s brilliant innovation in teaching as a new faculty member, including his ultra-modern insight about the value of integrating the biomedical sciences and the behavioral sciences coursework with the introduction of medical students into the poverty clinics. At the same time, he was envisioning curricular changes 50 years ahead of the mainstream, the energetic Richmond taught the biology of human development at the Institute of Psychoanalysis and lectured in Urbana weekly to students at the School of Social Welfare Administration (Bussey).
In the immediate post-war period, Richmond was funded as a Markle Scholar, which afforded him the opportunity from 1948-1953 to perform cutting edge research, characterizing the autonomic nervous system functioning of a variety of individual children (Palfrey). Richmond’s chronicler, Palfrey describes his groundbreaking work:
He was one of the first people to point out how infant brain growth depends on organized input from the external world. Before the advent of sophisticated brain imaging, he and his research colleagues documented the elaboration of synaptic connections in infants. He would demonstrate the intricate and vulnerable interactions of the newly forming brain, and he would take the next logical step to argue the importance of early cognitive stimulation. (Palfrey)
In 1953, Richmond departed UIC’s medical school to teach at the State University of New York at Syracuse College of Medicine and Chair of the Department of Pediatrics. While some historians suggest that Richmond and Caldwell were inspired by the Brown v. Board of Education case to study the influence of environment on childhood development (History of Medicine), a more critical analysis of Richmond’s transition by Bussey seems more likely and arises from his pedagogical differences with the UIC faculty leadership:
Two things prompted Richmond to leave the University of Illinois Medical School in 1953. Progressive in his views, he tried to move the medical school curriculum in a new direction. He wanted integrated teaching across departments, patient contact early in medical school, attention paid to psychological and social factors in health and illness, and emphasis on disease prevention and health maintenance. When the Executive Faculty of the medical school soundly defeated his proposal, and then failed to offer him the open Chair of the pediatrics department, Richmond began to consider other possibilities. Again, demonstrating his versatility and energy, Richmond was named director of the Institute of Juvenile Research, as well as continuing his teaching duties, during the year he remained in Chicago. Richmond disagreed with a colleague’s assessment that anti-Semitism had played a role in his disappointments, but he admitted he felt “somewhat bloodied by the faculty battle that had taken place.” His decision to leave Chicago in 1953, according to medical historian Patricia Spain- Ward, “was a sad day for the University of Illinois Medical School.” (Bussey)
Richmond styled the path of his lifelong adventure as “the incidence of coincidence,” and his biographer, Bussey rightly marveled at the “almost serendipitous convergence of historical forces and personal circumstances that shaped his career. Nowhere is that more profoundly demonstrated than by the move to Syracuse—and within a few years, Head Start” (Bussey). With hindsight, we may consider the roots of Richmond’s extraordinary path, and the modern reader might remember that the following brief highlights from Dr. Richmond’s career represent extraordinary and novel achievements in social medicine. Richmond accomplished his work on a grand scale.
At Syracuse, Richmond advanced his foundational studies of the developing child with psychologist Bettye Caldwell. At first, the pair assessed the development of the youngest of the urban poor, infants and toddlers, and were alarmed by the slowdown in learning by 18 months of children who had previously met basic milestones and were neither ill nor obviously impaired. Next, the colleagues started home visits and discovered that while the basics of survival were minimally present, there was very little in the environment to stimulate the children. Richmond and Caldwell developed an early childhood curriculum for impoverished preschoolers on their Syracuse campus. When they compared children exposed to the enriched environment with those who lacked exposure, the researchers found an enormous difference between the groups, demonstrating the effects of poverty (Palfrey).
The Johnson administration’s Great Society and War on Poverty was heating up in the mid 1960’s, accelerated by the appointment of Sargent Shriver as the new chief of the Office of Economic Opportunity (OEO). Shriver was interested in immediate action programs to lift families out of poverty. The story of Shriver’s invitation to Richmond to join the campaign is telling about the character of both men. Shriver, who never liked to wait, literally traveled to Philadelphia in order to send a note to Richmond at the speaker’s podium asking him to come to Washington. The note specified Richmond’s expected time of arrival to the new job as the next day (Bussey).
One historian of the Great Society, Davis defined the philosophy of social change shared by President Johnson who approved of Shriver’s choice in Dr. Richmond:
“Two men instrumental in the planning and implementing of the Great Society–President Lyndon Johnson and Dr. Julius Richmond, director of Head Start–agreed that certain societal factors had to be present before social change could occur. Johnson felt that these three conditions were “a recognition of need,” “a willingness to act,” and “someone to lead the effort” (Johnson The Vantage Point quoted by Davis).
Essentially, Shriver asked Richmond for the equivalent of a moonshot, a full-scale educational offensive on an impossible timeline. Palfrey, who has outlined Richmond’s three major contributions to public health, elegantly describes how Richmond achieved the first, the seemingly impossible lightning speed implementation of a program across the nation for 500,000 children at 3,000 locations
As the first national director of Head Start, Richmond traveled to small towns, rural villages, and big city neighborhoods throughout America. Over and over, he witnessed the same deprivation that he and Bettye Caldwell had encountered when they visited homes in New York State. He found children denied nurturing, children taken for granted, and children whose potential was being wasted.
He also found allies in the towns and cities, men and women who knew that the situation for young families could change. They recognized in Head Start a practical mechanism to turn things around but also knew that Head Start should invest in the community itself, should take advantage of the talents of local people. Under the umbrella of Head Start, these community leaders could introduce young children to language and song, pictures and stories about their heritage and their future. Years later Richmond would say that Head Start has succeeded so well because it rests on “contracts between the federal government and local communities, which have proved to be remarkably effective in giving people in local communities—and particularly parents—ownership and commitment for the health, education, and welfare of their young children.” (Palfrey)
Thus, Richmond achieved the first monumental pillar of his public health legacy with the Head Start program, which persists to this day, and has lifted up millions of children from impoverished environments. In the process of installing the Head Start network of centers across the country, Richmond also began to identify the systemic problems in the delivery infrastructure of healthcare for children. During the early days of Head Start, the seed was planted with Richmond for what Palfrey identified as his second great public health legacy:
As Richmond learned more about the needs and the strengths of communities, he identified gaps in the delivery of health care to young children. In the bayous and the backwaters, out where the tall wheat blew and in the swelter of the inner cities, Richmond recognized the dearth of easily accessible health care clinics for children. He was impressed by the ideas that community members brought to him. Richmond listened and responded with the kind of idea that Shriver could run with. How about a new type of community-organized, community-run health clinic? The OEO wanted to ensure the “maximum feasible participation of the poor.” What better way to create participation, ownership, jobs, and community health than to build and run these clinics? And so the neighborhood health center movement was born. (Palfrey)
In 1967, with the change of federal administrations, Richmond returned to Syracuse, where he was made Dean. In 1971, Richmond moved to Harvard, where he was appointed to lead two departments: the Department of Child Psychiatry and Human Development and the Department of Preventive and Social Medicine. A number of other responsibilities were taken up by Richmond in this period as he dedicated his energies to helping Boston’s children. Richmond led the Judge Baker Guidance Center (1971-1977) and was the Chief of Psychiatry at the Children’s Hospital” (History of Medicine).
In 1977, under President Jimmy Carter, Richmond accepted an invitation to return to government service on the condition he was appointed Surgeon General. Carter appointed Richmond as the 12th Surgeon General of the United States and Assistant Secretary for Health. Richmond began working toward the second pillar of his public health legacy with determination and using his diplomatic skills with the Congress. Legislation was passed to establish long-term federal funding of neighborhood health centers, which he had recognized as a necessity during the Johnson years and his travels across the nation for Head Start. His goal was realized in 1978 when Congress passed the Health and Human Services and Centers Act with a $3 billion dollar appropriation to build community and migrant centers as well as primary care centers and other community-initiated initiatives (Palfrey).
Richmond was masterful at using the tools of mass communication to achieve his goals. He convened a number of important stakeholder groups to create momentum for broad societal changes in healthcare. He issued the landmark public policy declaration in 1979, entitled “The Surgeon General’s Report on Health Promotion and Disease Prevention.” This Healthy People Report reflects Richmond’s genius as a strategic communicator and is still the major policy document informing our national and state public health agendas to this day. It represents Richmond’s third great legacy, according to Palfrey, and in some ways the most powerful since it engages several hundred broad aims in an evidence-informed strategic design. At this writing, the Healthy People Report has undergone several generations of revision and is an engine of public health transformation. Richmond used this report to reach out to the broad public, using media and local health departments, together with the national media, in order to influence and inspire the public’s interest in health promotion. By engaging the public and creating a standing strategic design instrument for forward movement, Richmond provided the infrastructure for healthcare research and policy agenda setting, which are foundational to change.
Part of Richmond’s public health legacy as Surgeon General also includes his efforts to advance life-saving public health change through tobacco control. Toward this end, he issued the famous 1979 report “Smoking and Health” (History of Medicine). In 1980, Richmond organized the “Workshop on Maternal and Infant Health.” The 75-person expert panel convened to develop a national strategy for reducing deaths and disparities in healthcare at the prenatal and pediatric levels (Heinz Awards).
When Richmond returned to Harvard in 1981, he was appointed as John D. MacArthur Professor of Health Policy and Director of the Division of Health Policy Research and Education. He served in these posts until he retired in 1988. As Professor Emeritus, Richmond’s retirement activities included service as the Steering Committee Chair for the National Academy of Science’s Forum on the Future of Children and Families. Richmond continued mentoring students and faculty as well as writing for years. He was an expert witness in the historical tobacco litigation. Then, in 1990, Richmond, the founding Chair of the AAP Section on Community Pediatrics and the Section on Child Development, received the American Academy of Pediatrics Excellence in Public Service Award (AAP website).
The Harvard School of Public Health’s highest honor, the “Julius B. Richmond Award,” was established in 1997.
On July 27, 2008, Dr. Richmond died of cancer at age 91. Professor Jack P. Shonkoff, the Julius B. Richmond FAMRI Professor of Child Health and Development and the Director of the Center on the Developing Child provided the following note on Dr. Richmond’s legacy: “Julie Richmond was an intellectual giant and a social activist with a gentle spirit. Through public example and personal relationships, he inspired thousands of leaders who have made the world a better place for millions of children” (Harvard, Obituary for Dr. Richmond).
Readers may wish to see some of the appearances of Dr. Julius Richmond available on YouTube. They are remarkable for both his gentle humor and great humility.
Works Cited
- American Academy of Pediatrics (AAP website). Dr. Julius B. Richmond (1916-2008). Accessed May 2020 at: https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Richmond-Center/Pages/Dr–Julius-B–Richmond-(1916-2008).aspx
- Bussey, C. J. (1993). Julius B. Richmond and Head Start: The dream become reality. Perspectives in Biology and Medicine, 36(3), 429-441. doi:10.1353/pbm.1993.0050. Accessed May 2020 at: https://muse.jhu.edu/article/401041/summary
- Davis, J. (1994). Prelude to the Great Society: Cultural Change in the 20th Century America. Student Honors Theses, 78. Accessed May 2020 at: http://digitalcommons.wku.edu/stu_hon_theses/78
- Harvard T.H. Chan School of Public Health obituary for Dr. Richmond (2008). “Julius B. Richmond, former U.S. Surgeon General and Professor of Health Policy, Emeritus, dies.” Harvard School of Public Health website, accessed May 2020 at: https://www.hsph.harvard.edu/news/press-releases/julius-richmond-former-us-surgeon-general-dies/
- Heinz Award website accessed May 2020 at: http://www.heinzawards.net/recipients/julius-richmond
- History of Medicine. Julius Richmond Papers. Biographical Note. National Library of Medicine website. Accessed May 2020 at: https://oculus.nlm.nih.gov/cgi/f/findaid/findaid-idx?c=nlmfindaid;idno=richmond383;view=reslist;didno=richmond383;subview=standard;focusrgn=bioghist;cc=nlmfindaid;byte=35360724
- Palfrey, J. (2006). Child health in America: Making a difference through advocacy. JHU Press. ProQuest Ebook Central. Accessed May 2020 at: http://ebookcentral.proquest.com/lib/uic/detail.action?docID=3318369.
-
David Sackett, MD (1934-2015)

David Sackett is considered a founder of the discipline of evidence-based medicine and was at the forefront of developing the medical education strategy of problem-based learning. After graduating from the University of Illinois college of medicine in 1960, he became interested in how methods of epidemiology could be applied to healthcare questions about the diagnosis, prognosis, etiology, and treatment of clinical problems.
At age 32, he became the founding chair of an innovative Department of Clinical Epidemiology and Biostatistics at McMaster University. He served as a mentor to many future scholars. Said one mentee, “He said to me, ‘My job is to make sure you meet your goals and objectives, and I will facilitate that for you….That’s exactly what he did. He didn’t do it for his career, because he already had a fantastic career. He just wanted to support young people.” (Collier)
Achievements
- Sackett was the first head of the first department of Clinical Epidemiology and Biostatistics in the world at McMaster University
- 1970-Sackett created a graduate program to teach clinicians and others how todo healthcare research
- 1993-Sackett became the first Chair of the Cochrane Collaboration Steering Group
- Sackett published 12 books, 60 chapters, and an estimated 300 papers in medicine
Full Bio
Dr. David Sackett was born November 17, 1934, to DeForest and Margaret Sackett (nee Ross). Sackett described his early life to Brian Haynes, one of his PhD mentee, in an interview close to the end of his life:
…I grew up in a small, semi-rural suburb of Chicago, the 3rd son of a bibliophile mother and artist-designer father. I remember our large Victorian house as filled with love, neighborhood kids, border collies, bagpipe and classical music, and books for every age and interest. My eldest brother became a Madison Avenue publishing magnate and the 2nd, a Stone Age archaeologist who became Chair of Anthropology at UCLA.
Because everything is ‘normal’ to a naïve kid, I enjoyed friendships with both black and white kids in our integrated schools, but raised no objections to my hometown’s racially segregated housing until my later civil rights days. I look back on my childhood as a happy time in a happy family.
I was a prototypical geek: far taller and skinnier than my classmates, my baseball aspirations shattered by monocular vision from severe amblyopia, my shyness exacerbated throughout 8 years of dental braces, and out of commission for half of my 12th year from polio and a post-polio leg contracture. (Sackett)
Sackett’s friend, Richard Smith, editor of the BMJ, commented on the lasting imprint of his childhood, “He lived in such houses all his life and was always a voracious reader” (Smith). In a revealing anecdote about his second-grade teacher’s forecast of Sackett’s lifelong temperament, echoes of Twain’s Tom Sawyer can be heard:
An enthusiastic student, I loved school, and couldn’t stop talking, joking and punning about it, especially in class, especially when I was supposed to be silent. After banishing me to the hall for much of grade 2, my teacher told my mom “Your boy will wind up either President of the United States or hung in a village square.” (Sackett)
New York Times writer, Sam Roberts, reported on what Sackett made of his early adversity: “Bedridden for months as a child with polio, David recovered and exercised to develop into an accomplished runner. He also became a voracious reader and, he said, the youngest member of the Society for the Preservation and Encouragement of Barber Shop Quartets Singing in America…” (Roberts). Toward the end of his life, Sackett reflected that he felt the polio was a “blessing.” Sacket completed high school at age 16, a year ahead of his class. Since he was too young to go onto college, he took another year of science and choir and kept up with the track team (Sackett).
Sackett attended the small, liberal arts Lawrence College in Wisconsin. In fact, so did his wife and both of his brothers and their future wives. At Lawrence, Sackett discovered his love for science but was conflicted about pursuing zoology or physiology. In the end, Sackett’s consultations with teachers and friends convinced him that becoming a physician was the way to deepen his understanding of physiology and “combat its derangements.” Sackett left Lawrence with Barbara Bennett who would become his lifelong partner and wife (Sackett).
From 1956 -1960, Sackett attended the University of Illinois Medical School. In his interview with Haynes, Sackett’s recollections of medical school elicited mixed feelings. He recalled the hardships of being an impoverished medical student, and the goodness of Dr. Robert Pumper, a virologist who became his first professional mentor. Sackett was glad to be of service to the impoverished patients who visited Cook County Hospital, but he was disappointed with the curriculum, which seemed divorced from the clinical context. He felt disappointed that his superiors were unable to supply evidence for their medical decisions, and instead resorted to explanations like “that’s how we’ve always done it” or “that’s how the ‘experts’ say we should do it” (Sackett). Sacket described his “predilection for marching to a different drummer” since he was in high school (Watts). Eventually, his divergent thought processes were reflected in his clinical decision-making and “constantly offending conventional therapeutic wisdom” (Watts).
Toward the end of medical school, Sackett had a life-transforming experience treating a patient with hepatitis. At the time, the “conventional wisdom” recommended extended bed rest, but Sackett’s patient was adamantly resistant to this therapy. Searching for another therapy, Sackett discovered Dr. Tom Chalmers, a US Army gastroenterologist who conducted a randomized controlled trial on hepatitis in the Korean War field of operations. It was Sackett’s first encounter with high-quality trial evidence from a journal and he convinced his supervisors to successfully utilize the treatment Chalmer’s study demonstrated. At the time RCTs were quite rare. Sackett describes the change wrought by this experience:
My subsequent ‘clinical course’ was far from uneventful. I became a ‘trouble-maker’, constantly questioning conventional therapeutic wisdom, and offending especially the sub-specialists when they pontificated (I thought) about how I ought to be treating my patients. I had a stormy time in obstetrics, where I questioned why patients with severe pre-eclampsia received intravenous morphine until their respirations fell below 12 per minute. I gained unfavorable notoriety on the medical ward, where I challenged a consultant’s recommendation that I should ignore my patient’s diastolic blood pressure of 125 mm Hg “because it was essential for his brain perfusion.” (Sackett)
Sackett undertook his residency training at the University of Illinois Research and Education Hospital between 1960-1963. He trained in internal medicine and nephrology. During this residency period, he was offered and accepted a National Institutes of Health Research Fellowship in nephrology (Haynes).
In 1962, during the Cuban Missile crisis, Sackett was recruited by the United States Public Health Service and stationed in Buffalo at the Chronic Disease Research Institute. Smith summarizes the effect of Sackett’s 1963-1965 sojourn to Buffalo on the arc of his career: “…he met epidemiologists, was diverted from his career in bench science and became interested in how methods of epidemiology could be applied to his ‘first love’ clinical medicine” (Smith). Sackett remembered his career-defining insight and seminal question at Buffalo “…my growing understanding of the strategies and tactics of population-oriented epidemiology and biostatistics made me wonder whether they might be redirected to individual patient-encounters and improve my diagnostic abilities, my prognostic predictions, and my selection and application of therapeutic interventions” (Sackett).
From 1965 to 1966, Sackett was the Chief Teaching Fellow in Buffalo where he honed his sensibilities about how to relate to students, sometimes through painful trial and error. Sacket revealed to Haynes such a painful episode at Buffalo with the approximately 30 interns he supervised. From this we have gathered a sense of what guided Sackett to become a humble and forbearing mentor eventually:
Not all my educational efforts were appropriate. To teach my house staff to avoid costly but unnecessary lab tests, at [one] of their ‘grand rounds’ I asked an intern to describe the end-of-life care he had given a terminal cancer patient who was well-known to our service. After praising his compassionate care, I took a strip off him in public for the unnecessary lab bill he’d run up on the patient’s last day. I took him aside later to apologize, but he remained quiet and wary of me for months thereafter. Although lots of senior clinicians still practice ‘education through humiliation’30, I rejected it from that day forward. (Sackett)
In 1966, Sackett determined to take an additional course of study with Harvard’s School of Public Health in Boston. He attended under the GI bill and took his wife and 4 boys to live in student housing. Sackett reports that the Chair of Epidemiology at Harvard SPH, Brian MacMahon, met with him and “kindly took me under his wing.” Sackett followed MacMahon’s advice not to take an MPH, rather take epidemiology and biostatistics courses, supplement with research, and finish with an MSc. Thus, Sackett was guided toward a course of studies supportive of his clinical orientation.
At Harvard and MIT, Sackett met an abundance of new friends, participated in the Framingham Heart Study at Dr. Kannel’s invitation, and deepened his understanding of epidemiological research and curricular design. Sackett’s work in this period moved him away from curricula focused on public health broadly toward a clinical epidemiological approach concerned with clinical examination accuracy and harm-benefit ratio analysis for therapeutics. Sackett reflected on the trend of thought he came to at Harvard, which led him to the next position at McMaster University: “I began to think about clinical ‘cases’ that might be introduced into classroom settings to illustrate and solve relevant clinical problems in precision, accuracy, and efficacy” (Sackett).
In 1967, Sackett was recruited to establish an innovative department at the newly formed McMaster University medical school in Canada. Haynes summarized some of Sackett’s achievements in the leadership of this tremendously innovative department, which eventually supported an evidence-based medicine revolution across the world:
… at Harvard University, he learned the methods of “population-based” epidemiology and convinced himself and others that he should work on applying them to healthcare questions about the diagnosis, prognosis, etiology, and treatment of clinical problems. He was given a surprising opportunity to do so by the new medical school at McMaster University, where, at the age of 32, he became the founding chair of the department of Clinical Epidemiology and Biostatistics. As a member of the then small faculty, he contributed heavily to the pioneering problem-based curriculum, including integrating clinical epidemiologic principles into the health care problems that provided the stimulus and framework for learning.
In 1970, Sackett created a graduate program to teach clinicians and others how to do health care research. Now named the Health Research Methodology Program, it has trained and launched the careers of hundreds of clinical epidemiologists, biostatisticians, and health services and policy researchers.
He saw that the sound research being done to answer important clinical problems was likely to whither on the vine unless clinicians learned more about how to identify, interpret, and apply sound studies while quickly side-stepping weak studies. Initially, this newly defined set of clinical skills was called critical appraisal of the medical literature, but it soon became evidence-based medicine. (Haynes)
Smith tells a slightly more behind the scenes version of Sackett’s coming to McMaster at the invitation of John Evans, who was shaping his new medical school in Hamilton. The story, retold with Smith’s characteristic flair for narrative, conveys the Sackett’s wry humor and galloping optimism:
…in 1966 it was Holland who suggested Sackett to John Evans, who was starting a new medical school at McMaster University in Hamilton, Canada.
After getting a letter from Evans “out of the blue” Sackett went to visit him, but, he didn’t want to leave the US, was 32 years old, and had, he told me in an interview, “never done anything.” Evans contacted him because he wanted “a different kind of medical school” and wasn’t taken with the traditional public health people in Canada. Sackett didn’t want the job and so could be very frank. Evans asked him about what sort of department of social medicine and community medicine they should have in the new school, and Sackett answered “none.” His point was that all clinicians should be concerned about these issues. In fact Evans had already reached the same conclusion.
Evans’s next question was what sort of course should there be to teach medical students epidemiology and statistics. Again Sackett answered “none,” arguing that these disciplines needed to be taught within the clinical disciplines. “Otherwise it would be just as awful as everywhere else. The students would hate the faculty. The faculty would hate the students. And it would be a shambles.” Again it’s what Evans wanted to hear: there weren’t going to be any courses in anything, students would learn from the problems of patients. This concept of medical education had come from William Spaulding, a Toronto physician and internist who had thought deeply about medical education and was another of Sackett’s mentors.
As Sackett put it, Evans mistook “a novice for a sage” and asked him to come back for a second interview. Eventually Sackett was appointed and started in 1967, with the first students arriving in 1969. “I was scared,” Sackett said, “I was a kid, I’d never really had a research grant, my previous publications were on basic science, so who would want to come and work with me or give me money for research?” Yet he was ambitious. He recognized that being scared was not compatible with being a new chair in a new medical school. He needed to be “incurably optimistic, convinced that everything was going to be great, incredibly positive, and get his kicks out of the successes of others.” So Sackett displayed those characteristics and attracted outstanding staff and lots of money. The author Kurt Vonnegut, a hero of Sackett’s, says you become what you pretend to be, so be careful what you pretend. (Smith)
Thus, from 1966-1994, Sackett was at McMaster University, Hamilton, Ontario, Canada. Thoma recollects Sackett’s transformation from a reluctant US transplant to a Canadian embracing an entirely different healthcare system:
In his own words, he fell in love with Canada within the first 3 months after arriving at McMaster. Although Canada and the USA share a common border, same language, and generally the same culture, in the late 1960s Canada decided to follow a different course in terms of health care. It decided to adopt a universal health care system. Sackett was excited about the prospect of universal health care and all the other social support systems available in Canada then but not available in the slums of Chicago, Buffalo, and Boston, where he had worked before. (Thomas)
At the age of 49, Sackett’s dedication as a clinician for patients was on full display when he undertook a 2-year residency program because he was concerned about his skills being stale. Robert and Suzanne Fletcher relate Sackett’s belief in lifelong learning: “David took time to foster his own career in an unusual way. At age 49 years, he went back into a “retreading” medical residency. He already had been chief resident years ago but decided he was out of date clinically. After “retreading,” he was more active in clinical settings than he had been in years” (Fletcher). Following this retread training, Sackett was appointed the Hamilton Health Sciences Chief of Medicine (Haynes).
In 1993, Sackett became the first Chair of the Cochrane Collaboration Steering Group (“In Memoriam…”). At the invitation of Muir Gray and the National Health Service, Sackett then founded and directed the Oxford Centre for Evidence-Based Medicine in the UK in the 1994-1999 period. He also worked in Oxford as a clinician at the John Redcliffe Hospital. Sackett’s clinical work at the hospital and directorship of the Centre for Evidence-Based Medicine during the 1990’s was sometimes met with resistance. In an interview Sackett stated “The Establishment saw EBM as an affront to their omniscience and authority, and dismissed it as an ‘old hat’ (‘everybody’s already doing it’) and a ‘dangerous innovation perpetuated by the arrogant to serve cost cutters and suppress clinical freedom.’” (Sackett Interview). “During this period of controversy, a 1995 Lancet editorial was published, “Evidence based medicine, in its place.” The article was offensive to Sackett, who had been involved in the civil rights movement, because it evoked the familiar American phrase “black guys are OK, in their place” (Smith). Fortunately, history saw the place of evidence-based medicine expand.
Sackett was interested in spreading evidence-based healthcare practice and principles not just to Oxford but to the rest of the UK, Europe, and beyond. He visited most of the district general hospitals in the UK and many in Europe, and he would begin his visit by doing a “post-take ward round” with young doctors, showing evidence-based medicine in action. In 1998 he made 100 visits. The young doctors realized that they could challenge their seniors in a way that wasn’t possible with expert or authority-based medicine. It was liberating and democratizing. Smith relays the experience of another renown advocate of the evidence-based medicine movement:
Paul Glasziou, a general practitioner and professor of evidence based medicine at Bond University in Australia, 25 years later still remembers vividly a ward round with Sackett: a student used a decision aid to calculate the chances that a patient had an anemia and the clinicians consulted a systematic review on the value of treating the patient with ferritin. It was completely different from the traditional ward rounds he’d experienced. (Smith)
In 2000, Sackett returned to Canada to focus on teaching health research methodologies in clinician-oriented “Trout Workshops.” Smith points out that when he returned from Oxford, Sackett retired from clinical practice. He devoted his time at the Trout Research and Education Centre to reading, research, writing, and teaching (Smith). The objective of the Trout Workshops was to support graduate students and new faculty understand the principles of clinical epidemiology applied to clinical practice research (Sackett).
Haynes summarizes Sackett’s work as a teacher and his philosophy, “He estimated that he had mentored more than 300 students and colleagues during his career. He also taught his mentees how to mentor, creating a huge multiplier effect” (Haynes). In his memorialization of Sackett, Roger Collier wrote about Sackett’s students who are themselves among the stellar lights of teaching and EBM-conceptual framework development—clear proof of Haynes correctness in ascribing a “huge multiplier effect” to Sackett, the teacher of teachers:
It was not only his intellect, however, that attracted people to Sackett. That was but one of many traits that made him popular among those he took under his wing. “He was a wonderful mentor in terms of being a superb role model and in terms of critical thinking and kindness and skepticism and dedication and hard work and commitment, and he was great at bringing young people together and helping them work together,” said Dr. Gordon Guyatt, a distinguished professor in the department of clinical epidemiology and biostatistics at McMaster. “The other thing that he conveyed was that as hard as you work and as seriously as you take it, it should all be fun.” (Collier)
According to Collier, another of Sackett’s mentees, Sharon Straus, “was struck by his genuine interest in helping young physicians develop their careers.” Straus related her conversation with Sackett:
“He said to me, ‘My job is to make sure you meet your goals and objectives, and I will facilitate that for you’,” said Straus. “Nobody had ever said that to me and it was very empowering. And he lived it. That’s exactly what he did. He didn’t do it for his career, because he already had a fantastic career. He just wanted to support young people.” (Collier)
From 2000-2015, Sackett lived in Irish Lake, Ontario, Canada (Fletcher). During this period, he continued to have enthusiastic exchanges with his colleagues, friends and family. In 2001 he was made an Officer of the Order of Canada, which he styled as “the Canadian equivalent of a knighthood, but without the swordplay” (Daily Telegraph).
Sacket published 12 books, 60 chapters, and an estimated 300 papers in medicine (Smith).
Richard Smith writes warmly about his friend David Sackett in semi-retirement and at the end of his life:
A big, warm, and emotional man Sackett lived his final years with his wife, Barbara, in a wooden cabin beside a lake that was frozen for much of the year. Sackett always described himself as a man of the north. They had many family and friends to stay and would invite them all to canoe on the lake. Asked by students and colleagues for the reasons for his success, Sackett included among several reasons: “An insuppressible capacity for finding and injecting fun into everything I did (sometimes to the distress of others).” He also included “The enduring, loving support, encouragement, and understanding of Barbara and our four sons.” He leaves Barbara; four sons; and grandchildren. (Smith)
Peter Tugwell, who was Sackett’s student and remained close to him towards the end of his life, shared excerpts from Sackett’s note to him after his cancer diagnosis.
Now in our 80th years, we’ve repeated the calculus for the new cancer and its treatment options, and have again identified life-quality as the over-riding goal. All of this is made easier by our happiness and life-satisfaction; First, our kids are wonderful people, independent and happy; we have switched from ‘parenting’ to ‘doting.’ Second, I am simply delighted with what I’ve accomplished in my career, have had a wider range of experiences and opportunities than I could ever have imagined, working with brilliant/inspiring/loving and fun-loving colleagues like you, have been guaranteed immortality through the continuing accomplishments of the young people I have mentored, have no more axes to grind, and am not mad at anybody! I am at peace. Love and hugs, Dave.” (Tugwell)
Works Cited
- Collier, R. (2015). Dr. David Sackett, a giant among giants (1934-2015). CMAJ : Canadian Medical Association Journal = Journal De l’Association Medicale Canadienne, 187(9), 640-641. doi:10.1503/cmaj.109-5072. Accessed May 2020 at: https://www.cmaj.ca/content/187/9/640.short
- “David Sackett, physician – obituary: Pioneer of evidence-based medicine who showed aspirin has health benefits.” (2015). Daily Telegraph (London, England). Accessed May 2020 at: https://www.telegraph.co.uk/news/obituaries/11630337/David-Sackett-physician-obituary.html#:~:text=Pioneer%20of%20evidence%2Dbased%20medicine%20who%20showed%20aspirin%20has%20health%20benefits&text=David%20Sackett%2C%20the%20physician%2C%20who,prevent%20heart%20attacks%20and%20strokes.
- Fletcher, Robert H., and Suzanne W. Fletcher. “David Sackett was one of a kind.” Journal of clinical epidemiology 73 (2016): 67-72. Access May 2020 at: https://search.proquest.com/openview/5ea602a335a3d294ef7c5e536e7242b9/1?pq-origsite=gscholar&cbl=105585
- Haynes R. B. (2015). ACP Journal Club: David Lawrence Sackett, MD, MSc (Epidemiology), 1934-2015. Annals of internal medicine, 163(4), JC2. Accessed May 2020 at: https://doi-org.proxy.cc.uic.edu/10.7326/ACPJC-2015-163-4-002
- “In Memoriam: Dr David Sackett, Founding Chair of The Cochrane Collaboration.” In Memoriam: Dr David Sackett, Founding Chair of The Cochrane Collaboration | Cochrane Canada. Accessed May 2020 at: https://canada.cochrane.org/news/memoriam-dr-david-sackett-founding-chair-cochrane-collaboration
- Roberts, Sam. May 19, 2015. “Dr. David Sackett, Who Proved Aspirin Helps Prevent Heart Attacks, Dies at 80.” Accessed May 2020 at: https://www.nytimes.com/2015/05/20/us/dr-david-sackett-who-proved-aspirin-helps-prevent-heart-attacks-dies-at-80.html?_r=0
- Sackett, D. L. (2016). interview in 2014-2015. Accessed May 2020 at: https://www.bmj.com/content/bmj/suppl/2015/05/18/bmj.h2639.DC1/David_L_Sackett_Interview_in_2014-15.pdf
- Smith, R. (2015). David Sackett. BMJ: British Medical Journal, 350. Retrieved May 2020 at: www.jstor.org/stable/26519887
- Thomas, A., & Eaves, F. F. (2015). A brief history of evidence-based medicine (EBM) and the contributions of Dr David Sackett. Aesthetic Surgery Journal, 35(8), 261-263. doi:10.1093/asj/sjv130. Accessed May 2020 at: https://academic.oup.com/asj/article/35/8/NP261/251339
- Tugwell, P. (2016). David Lawrence Sackett (DLS) 1934–2015. Journal of Clinical Epidemiology, 69, 1-4. doi:10.1016/j.jclinepi.2015.09.012. Accessed May 2020 at: https://www.jclinepi.com/article/S0895-4356(15)00438-2/fulltext
- Watts, G. (2015). David Lawrence Sackett. The Lancet, 385(9985), 2348. Accessed May 2020 at: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)61094-7/fulltext
-
José Choca, MD (1959-1994)

Dr. José Ignacio Choca was born in 1959 in Havana, Cuba. His family, including 5 siblings, migrated to the US when Choca was still an infant. After earning his bachelor’s degree at Johns Hopkins University, Choca received his MD/PhD from the University of Illinois College Of Medicine. He took great pride in his work to help minority medical students continue in school. In addition, he tutored international medical graduates for medical board exams. Choca’s advocacy for the primacy of teaching in universities was reflected in his 1992 letter to the Chicago Tribune, wherein he took issue with the bias toward research over teaching in government sponsorship and university culture.
His passion for research on sensory pathways and teaching continued despite learning he was HIV+ in 1991. He died of complications of AIDS in 1994 at the age of 35.
Achievements
- Dr. Choca was a 3-time winner of the Golden Apple Award at the University of Illinois in his 5 years on faculty. This award is based on students‘ election of a teacher that exemplifies the highest standards in education.
- 1994- Dr. Choca was posthumously awarded the Alpha Omega Alpha (AΩA)Robert J. Glaser Distinguished Teacher Award from AAMC. This highly prestigious award is given to only one of 4 faculty in the nation annually.
Full Bio
Dr. Jose Ignacio Choca was born in 1959 in Havana, Cuba. His family, including 5 siblings, migrated to the US when he was still an infant. After earning his bachelor’s degree at Johns Hopkins University, Choca was accepted into the combined MD/PhD program at the University of Illinois College of Medicine, obtaining his MD and a PhD in pharmacology in 1988 (Heise). As a medical student, Choca was the runner-up for the 1988 Osler Medal, an annual competition sponsored by the American Association for the History of Medicine for the best essay on a historical medicine topic. Choca’s essay was entitled, “A mode of action: historical aspects of the receptor theory” (AAHM).
Following his graduation Dr. Choca joined the UIC faculty as an assistant professor in the Department of Pharmacology, working with his former thesis advisor, Herbert K. Proudfoot, on the role of catecholamines in pain perception within the nervous system. He was especially talented as a teacher, winning a Golden Apple Award – by vote of the medical students – three times during his all-too-brief career. He was also devoted to the mentoring of students from foreign health professions programs, assisting them in their preparation for board examinations. Choca’s advocacy for the primacy of teaching in universities was reflected in a 1992 letter to the Chicago Tribune; he took issue with the bias toward research over teaching in government sponsorship and university culture. (Heise)
Dr. Choca died in August 1994 at St. Joseph Hospital at the age of 35, from complications of HIV/AIDS. Dr. William Wallace, dean of students at the College of Medicine, was quoted in a Tribune obituary, saying that “He was brilliant, and he loved teaching and working with students… As he became sick and was in the hospital, his students kept coming back to thank him…” (Heise). In that same year, he received (posthumously) the Alpha Omega Alpha Robert J. Glaser Distinguished Teacher Award from the Association of American Medical Colleges, then and to this day the most prestigious honor in American medical education specifically intended for teachers of medical students (AAMC).
The Latino Medical Student Association at the College of Medicine sponsors a scholarship named in his honor (Student Activities web page).
Sources Cited
- Heise, K. (1994). Dr. Jose Choca; 3-time winner of UIC Prof Award. Chicago Tribune. Accessed May 2020 at: https://www.chicagotribune.com/news/ct-xpm-1994-08-27-9408270174-story.html
- American Association for the History of Medicine. Past Osler Medal Winners. Accessed May 2020 at: https://www.histmed.org/past-osler-medal-winners
- Association of American Medical Colleges. Alpha Omega Alpha Robert J. Glaser Distinguished Teacher Awards Recipients. Accessed July 2020 at: https://www.aamc.org/what-we-do/aamc-awards/aoa-glaser-distinguished-teacher/recipients
-
Arno Motulsky, MD (1923-2018)

Arno Motulsky was born in Germany to Jewish parents. He came to the United States in 1941 as a refugee from Nazi Germany, after first being sent to an internment camp in Vichy France. He worked his way through night classes to obtain his GED, then joined the US Army. In 1944, he began medical school at the University of Illinois as a soldier, private first class.He became a hematologist and physician-scientist, initially studying sickle cell hemoglobin. In 1957, he was asked to establish a Division of Medical Genetics at the University of Washington. There, he founded the field of pharmacogenetics. He mentored hundreds of fellows and students over 50 years, including 1985 Nobel Prize winner Dr. Joseph Goldstein.
Achievements
- Arno Motulsky authored in excess of 400 articles, including the definitive text book of his field for its time, Human Genetics: Problems and Approaches, co authored with Friedrich Vogel
- Dr. Motulsky was the recipient of some of the most distinguished honors awarded in medicine, including awards from the National Academy of Medicine, the National Academy of Sciences, and the American Philosophical Society
Full Bio
Arno Motulsky was born in Germany on July 5th, 1923 to Jewish parents, Herman and Rena (nee Sass). Hermann was a shopkeeper in the town of Fischhausen on the Baltic Sea. Motulsky recounts a happy childhood and early enjoyment of reading and school. As a teenager, he developed a fascination with “what makes people tick,” and contemplated a career in psychiatry and psychoanalysis (Motulsky & King).
As the Nazi regime gained power in the later 1930’s, the Motulsky’s determined it was necessary to leave Germany and go to Chicago where Hermann’s brother was living. The father went to Cuba where he hoped to get visas for the family to enter the United States. However, by 1939, the family was still waiting as Germany grew increasingly dangerous. It was decided that Rena and the children should meet the father in Cuba and wait for the permits. At age 16, Motulsky went with his mother and younger siblings, together with more than 900 Jewish refugees on the ship MS St. Louis*, leaving Hamburg for Havana. Cuba, however, did not allow the passengers to disembark, giving the reason that the entry cards were invalid (Motulsky, 2018).
Motulsky tells the story of passengers aboard the St. Louis as it made its way back to Germany:
So ultimately the ship had to return to Europe. I was 16, so still a little naive, but many of the passengers had been interned previously and knew what awaited us on our return. Some attempted suicide by jumping overboard. Telegrams were sent all over the world asking that we be allowed to disembark anyplace other than Germany. Miraculously, a few days before we would have arrived back in Germany, four other countries—England, France, Holland, and Belgium—each agreed to take one-fourth of the passengers. By luck of the draw, my mother and brother and sister and I were assigned to Belgium. So in June 1939, I started high school in Brussels. (Motulsky & King)
The Motulsky’s went to Belgium, but when the Germans invaded several months later, Arno was arrested as an “enemy alien.” The young man was sent to internment camps run by the French Vichy government in St. Cyprien and Gurs, France. Motulsky relates, “the internment camps had no food or sanitation. Many prisoners died, most from typhoid or starvation” (Motulsky & King). Fortunately, Motulsky had acquired a United States visa at some point and was eventually allowed to go to a camp near an American consulate. Although his visa was expired, he persuaded the authorities to renew it, and he left for Spain and then Lisbon, in June 1941. It was just 10 days before his 18th birthday, and it is reported that if had turned 18 in France, he would not have been allowed to go to Spain. Instead, he would have been taken into Gestapo hands a few months later when the Vichy turned over the camps (Motulsky & King).
*The reader may be interested to know the ship bearing the Motulsky family has been the subject of film (e.g. “Voyage of the Damned,” 1976), plays, and books because of the harrowing events the passengers experienced and the eventual deaths of many who were returned to Nazi occupied territory. Readers may also be interested to research more about groups in the United States and Canada who played a part in turning away this ship and its desperate company.
Motulsky sailed to the United States, arriving in August 1941. He joined his father, but it was not until 1946, that his mother and siblings were able to make their way from Switzerland to Chicago. Between 1941 and 1943, Motulsky accomplished an amazing series of life milestones: he finished his high school GED in night classes, he started college at the Central YMCA College (later Roosevelt University), he applied and was accepted to medical school at the University of Illinois, he became a US citizen, he joined the US army, and he met his future wife, Gretel who was also a refugee. In 1943, Motulsky also was sent to Yale by the army to complete premedical classes in a rapid development program for young physicians. Motulsky describes the happiness and productivity of this whirlwind period.
Yale was fantastic! I walked into Sterling Library, looked up and around, and thought I’d died and gone to heaven. The next year at Yale was a tremendous experience. I took genetics with Donald Poulson and was hooked forever. I finished the premed courses at Yale at the end of 1943, and in the three months before medical school started back in Chicago, was assigned as an orderly to an army hospital near Boston. In April 1944, I began medical school at the University of Illinois as a soldier, private first class. I was released from the army in 1946 at the end of the war, finished medical school in 1947, and took a residency in internal medicine and a fellowship in hematology at Michael Reese Hospital in Chicago. (Motulsky & King)
Motulsky’s fellowship at Michael Reese was supervised by Dr. Karl Singer and focused on sickle cell hemoglobin through the lens of rabbit immunology. When the Korean War begin in 1951 and Motulsky re-enlisted, he was assigned to the start-up hematology unit at Walter Reed Hospital in Washington DC. As a result, Dr. Motulsky conducted a number of the first successful experiments on structural anemias. Because of this work, in 1953, Motulsky was offered a choice between the highly competitive William Castle fellowship at Harvard and an internal medicine appointment at the University of Washington, where he was to establish a Division of Medical Genetics in 1957. Motulsky chose the adventure of Seattle. In preparation for his new role, Motulsky spent a year working with the foremost scientists in the emerging new field of medical genetics. Here is his recollection:
Before starting a Division of Medical Genetics, I needed to learn what was possible. Jim Neel’s department at Michigan was the most exciting human genetics program in the country. Jim was a geneticist with tremendous breadth and depth in the field who had gone to medical school after completing his PhD (39). He realized that the province of medical genetics extended all the way from physiology to populations and embraced areas, like statistical genetics, outside his immediate expertise. He became my mentor and role model, although he was only seven years older than me. In order to bring Jim’s broad perspective to Seattle, I needed to know more about mathematical genetics. So I spent eight months in the human genetics unit of Lionel Penrose at University College London (10). Penrose’s department was the best in human genetics in Europe, including, in addition to Penrose himself, J.B.S.Haldane, C.A.B. Smith, and several others. People were very critical and helped me recognize excellent work. (Motulsky & King)
In his memorial essay, John Opitz summarizes some of Motulsky’s achievements, which reflect both his service to the nation and its investment in him:
Rarely, in our field, has anyone taken on higher teaching and investigative responsibilities with greater talent or didactic qualifications than Arno G. Motulsky. The investment by the U.S. Army in his education paid off in almost 60 years of service to the University of Washington, the establishment of an important new branch of biological science (Pharmacogenetics), of a world-class training program (48 postdocs, the standard textbook in the field), and of a highly successful, productive research program leading to a Nobel Prize… addressing one of the most urgent health problems of humankind—the lipid defects predisposing to myocardial infarcts. (Opitz)
George Stamatoyannopoulos, who called Arno “a great intellectual and a great friend” recounted some of Dr. Motulsky’s many professional associations and distinctions:
He was a member of the American Society for Clinical Investigation, the Association of American Physicians, and the American Philosophical Society. The American Society of Human Genetics honored him with all three of its major awards: the William Allen Memorial Award, the Excellence in Education Award, and the Victor A. McKusick Leadership Award, and it established in his honor the Arno Motulsky–Barton Childs Award for Excellence in Human Genetics Education. (Stamatoyannopoulos)
Dr. Motulsky authored in excess of 400 scientific articles, and the definitive textbook of his field for its time together with Friedrich Vogel. He was also the recipient of some of the most distinguished honors awarded in medicine, including awards from the National Academy of Medicine, the National Academy of Sciences, and the American Philosophical Society (Grady).
New York Times reporter, Denise Grady characterized Motulsky’s achievements in the words of his colleagues and mentees, who recognized his visionary influence over the infant field of genetics. For example, Francis Collins acknowledged Motulsky’s groundbreaking contribution to the field of Pharmacogenetics, which investigates the effect of individual genotypes on patients’ responses to drugs:
It was his vision to study how heredity could be involved in practically everything,” Dr. Francis Collins, a geneticist and the director of the National Institutes of Health, said in an interview. “The relationship between heredity and the response to drug therapy — nobody was thinking about that until he started, 60 years ago. He anticipated it decades before science made it possible to get the answers that he dreamed of.” (Grady)
Dr. Mary Claire King, a leading geneticist at the University of Washington who discovered linkages between breast cancer and genetics, lauded the Motulsky’s broad engagement of population genetics and diseases: “…the field is now integrated into every other field of medical practice, and has become the soul of precision medicine” (Grady).
One of Motulsky’s most notable mentees, Joseph Goldstein, won a Nobel Prize in 1985 for his work on cholesterol reducing drugs. Goldstein expressed his gratitude for Motulsky’s support and encouragement, which greatly facilitated his Nobel work:
“Arno was sort of a maestro of human genetics,” Dr. Goldstein, now chairman of the department of molecular genetics at the University of Texas Southwestern Medical Center in Dallas, said in an interview. He added in an email, “He gave me the confidence to design a large study on lipid levels in survivors of heart attacks and gave me support and resources — at a time when I was only 28 years old.” (Grady)
In his semi auto-biographical article (“as story told to Mary Claire King”), Dr. Motulsky shared his sense of achievement as a mentor and teacher through his textbooks, stressing the importance of well-formed questions and research projects that press into new discovery:
I believe that my most important contribution to medical genetics has been mentoring hundreds of fellows and students over the past 50 years, and I was delighted when my way of mentoring became a model for the field (31). Part of mentoring, including reaching young scientists I don’t know personally, has been writing textbooks that present our field in all its complexity and elegance. Between 1979 and 2010, Friedrich Vogel and I wrote four editions of Human Genetics: Problems and Approaches (51). The text has appeared in English, German, Italian, Russian, Japanese, and Chinese. We present genetics as a series of problems for readers to think about, applying approaches from medicine, biochemistry, statistics, and most recently genomics to their solution. In advising young fellows how to select a research problem, whether by example from the text or from clinical work or from an experimental observation, my theme is that a good problem pushes knowledge ahead. It does not just add another brick to the edifice. In practical terms, it’s probably a good idea to have several projects in play at the same time. The most fun are Sunday morning projects, to work on when no one else is around. Sunday morning projects are less likely to work, but ultimately a few may really change the field. What will be good problems for the next generation of geneticists? With the completion of the Human Genome Project, we now have the table of genes, just like the table of elements. We can answer genetics questions much more rapidly than in the past, but the fundamental questions themselves have not changed. I think the next great challenge will be to understand how gene products interact with each other and with nongenetic factors. Genetics is linear, but these problems have more dimensions. (Motulsky & King)
Jarvik and King, Motulsky’s longtime colleagues remember the long line of his mentorship to geneticist who would eventually become world leaders themselves, and his openness to diversity:
“Many other medical geneticists were not formally his trainees but learned from him in conversations and in clinics. Links to Arno as a teacher appear wherever one touches down in medical genetics. We think it likely that Arno has mentored, formally or informally, a large proportion of medical geneticist now practicing in this country and abroad. As with other founders of our field, Arno welcomed women and men and young scientists of all ancestries as trainees. The diversity of our field is a tribute to this inclusive welcome. (Jarvik & King)
Another Motulsky trainee, Dr. Debra Freedenberg, Medical Director of the Newborn Screening and Genetics Unit for the Texas Department of State Health Services applauded her mentor’s efforts to include minorities: “Having started [a] genetics fellowship at a time when women in medicine were relatively rare, Arno was truly gender blind, wanting only the best training for those he mentored” (Jarvik, 2018). Dr. Motulsky’s characteristic ethical sensitivity to bias and ethnic discrimination was also alluded to in Oransky’s obituary for him in the Lancet:
Late in his career, Motulsky acknowledged that the field he helped create raised difficult questions. “Any discussion of population origins raises the question of whether the term ‘race’ is meaningful in genetics. I am uncomfortable with the term, because of the horrible misdeeds that have been done in its name.” Ultimately, he said, “with respect to genetic ancestry, race is less important than a patient’s genotype at any specific alleles that influence sensitivity to disease or to a drug.” (Oransky)
Motulsky’s intellectual stamina was matched by his dedication to people, as reflected in his long clinical practice and love for his family. In his autobiography, Motulsky talked his enjoyment of active service as an attending in internal medicine until he was 70 years old. Most beautifully, Dr. Motulsky also celebrated his life companion, wife and mother of his 3 children, Gretel, who pre-deceased him in 2009: “I was only able to do all that I did because Gretel took care of everything: our home, our children, and me. And she made it look easy. She was amazing. I was incredibly lucky to have found, early in my life, a partner of such intelligence, humor, and spirit” (Motulsky & King).
Dr. Motulsky was actively engaged with professional meetings and activities until 92 years of age. He passed away at age 94 in Seattle on January 17, 2018. John Opitz wrote a tender memorial for his friend and colleague of over 40 years for the American Journal of Medical Genetics:
This, in brief outline, is the story of Arno G. Motulsky, not finished, only begun. A heroic story it is of a truly fortunate man, fortunate to have survived the deadly anti-Semitism of Hitler in his native Germany, the Nazi invasion of Belgium, and the internment camps of Vichy, France, and to end up in Chicago in one piece and with an intact family, unlike most other European Jews and Jewish families. I cannot but wonder to what extent Arno’s most admirable personality and character traits, his integrity and honesty, kindness and humility, drive and commitment to the highest standards, openness to the new, indeed the very catholicity of his interests were innate or acquired during his first 16 years in Fischhausen? We will never know, but what we do know is sufficient to inspire future generations to redeem their suffering and to bestow meaning on their existence in like manner and with like generosity, tolerance, and good grace. (Opitz)
Works Cited
- Grady, D. (2018, ). Arno Motulsky, a founder of medical genetics 60 years ago, dies at 94: Obituary (obit); biography. New York Times. Accessed May 2020 at: https://www.nytimes.com/2018/01/29/obituaries/arno-motulsky-dies-medical-genetics-founder.html#:~:text=Motulsky%2C%20a%20former%20refugee%20from,%2C%20Harvey%2C%20confirmed%20the%20death.
- Jarvik, G. P., & King, M. (2018). Arno G. Motulsky (1923–2018): A founder of medical genetics, creator of pharmacogenetics, and former ASHG president. The American Journal of Human Genetics, 102(3), 335-339. doi:10.1016/j.ajhg.2018.02.005. Accessed May 2020 at: http://scholar.google.com/scholar_url?url=https%3A%2F%2Fwww.cell.com%2Fajhg%2Fpdf%2FS0002-9297(18)30050-8.pdf&hl=en&sa=T&oi=ggp&ct=res&cd=0&d=12427021317305742449&ei=nqDxXrupE6aA6rQPgLm6uAE&scisig=AAGBfm38UPKA-mybcUMTF3fqy4Mtw-KHaA&nossl=1&ws=769×581&at=Arno%20G.%20Motulsky%20(1923%E2%80%932018)%3A%20A%20founder%20of%20medical%20genetics%2C%20creator%20of%20pharmacogenetics%2C%20and%20former%20ASHG%20president
- Jarvik, G. P. (2018). Arno G. Motulsky, MD (1923-2018): Holocaust survivor who cofounded the field of medical genetics. Genetics in Medicine : Official Journal of the American College of Medical Genetics, 20(5), 477-479. doi:10.1038/gim.2018.55. Accessed May 2020 at: https://www.nature.com/articles/gim201855
- Motulsky, A. G. (2018). A German‐Jewish refugee in Vichy France 1939–1941. Arno Motulsky’s memoir of life in the internment camps at St. Cyprien and Gurs. American Journal of Medical Genetics Part A, 176(6), 1289-1295. doi:10.1002/ajmg.a.38701. Accessed May 2020 at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6001526/
- Motulsky, A. G., & King, M. (2016). The great adventure of an American human geneticist. Annual Review of Genomics and Human Genetics, 17(1), 1-15. doi:10.1146/annurev-genom-083115-022528. Accessed May 2020 at: https://www.annualreviews.org/doi/full/10.1146/annurev-genom-083115-022528
- Opitz, J. M. (2018). Arno G. Motulsky, 1923–2018, luck and service. American Journal of Medical Genetics Part A, 176(6), 1285-1288. doi:10.1002/ajmg.a.38702. Accessed May 2020 at: https://onlinelibrary.wiley.com/doi/abs/10.1002/ajmg.a.38702
- Oransky, I., & Marcus, A. (2018). Arno Motulsky. The Lancet, 391(10136), 2207-2207. doi:10.1016/S0140-6736(18)31167-X. Accessed May 2020 at: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31167-X/fulltext
- Stamatoyannopoulos, G. (2018). A tribute to Arno Motulsky. The Journal of Clinical Investigation, 128(5), 1709-1710. doi:10.1172/JCI121197. Accessed May 2020 at: https://www.jci.org/articles/view/121197
-
Rivers Frederick, MD (1874-1954)
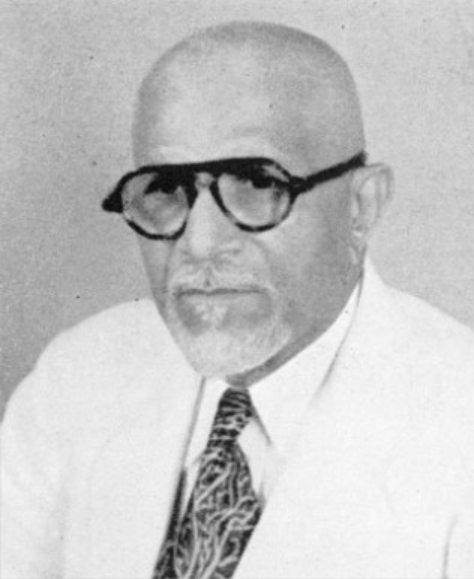
In 1897, Frederick became the first African American to graduate from the new Chicago College of Physicians and Surgeons (UIC) with a medical degree. He then won a highly competitive 18-month scholarship to the John B. Murphy Surgical Clinic at Cook County Hospital in Chicago, based on his examination scores. in 1899, Frederick returned to Louisiana because of his” growing desire to return to the place of my birth in order to help train young Negroes for adequate service in the growing field of medical practice, badly needed among our people.” At the time, it was rare for black physicians to return South, but Frederick joined the less than 50 African American physicians in Louisiana who cared for the state’s Black population of half a million. In 1908, Frederick accepted the post of Chief Surgeon at Sarah Goodridge Hospital in New Orleans and in 1932 took up the position of Chief of Surgery at the Flint-Goodridge Hospital at Dillard University. He played an instrumental role in the formation of the local NAACP Branch and remained a life member. Despite his great accomplishments, for many years Frederick was denied membership to both the American College of Surgeons and the International College of Surgeons because of racism.
Achievements
- 1923- Frederick became one of the founders of the black-owned Louisiana Life Insurance Company, known today as the Universal Life Insurance Company. Frederick filled the roles of a board member, secretary, vice-president, and president
- 1934- Frederick became the first vice-president of the National Medical Association
- Award of Merit for Outstanding Service- The American Cancer Society
- 1949- Honorary presidency of the New Orleans Urban League
Full Bio
Dr. Rivers Frederick was born May 22, 1874 to George Frederick and Armantine Dalcourt. Rivers grew up in a large Creole family of twelve children on the Drouillard Plantation in Pointe Coupee, Louisiana. At age 26, Frederick left the plantation and enrolled in New Orleans’s historically black college, Straight University (later Dillard University).
In 1894, Frederick graduated from Straight University and matriculated at the Medical College of New Orleans. Frederick’s training in New Orleans was interrupted, however. In 1896, Dr. Frederick left New Orleans and continued his education at the College of Physicians and Surgeons in Chicago (known today as the UIC college of medicine). Frederick’s change in schools was motivated by the need to study in a hospital that admitted black medical students. Since black medical students were not permitted to study in hospitals in New Orleans, Frederick made the journey north to Chicago. In 1897, Frederick became the first African American to graduate from the new Chicago College of Physicians and Surgeons with a medical degree. He then won a highly competitive 18-month scholarship to the John B. Murphy Surgical Clinic at Cook County Hospital in Chicago, based on his examination scores. Up to this time, Rivers Frederick had financed his education exclusively with the help of family members and by tutoring (Cherrie).
During this post-graduation period, Frederick married a white woman, Adele Boui, and purchased a 210-acre plantation in Louisiana. In 1899, after completing his 2-year surgical internship, he returned to practice medicine in Louisiana (DeCuir). At the time, it was rare for black physicians to return South, but Frederick joined the less than 50 African American physicians in Louisiana who cared for the state’s black population of half a million. On his return, Frederick became the parish doctor for a mixed-race practice, and was welcomed by patients in the community. However, Frederick’s marriage was treated with hostility by some members of the white community, and he was forced to travel to Spanish Honduras to continue his practice. In Central America, he became surgeon-in-chief for a government facility. Unfortunately, the physician contracted malaria and eventually planned his return to the United States. Significantly, when Frederick came back to Louisiana after 4 years, he relocated to New Orleans and eschewed Pointe Coupee (Cherrie).
After his return to New Orleans (between 1904-1906), Frederick became an Associate Professor of Surgery at Flint Medical School, where he stayed until 1908. Frederick’s first wife, Adele gave birth to their first of their 2 children, Pearl, on June 18, 1906. In 1908, Frederick accepted the post of Chief Surgeon at Sarah Goodridge Hospital in New Orleans, where he remained until 1913. In this period, his second daughter, Lolita, was born (June 27, 1911) (Amistad Research Center website).
In 1923, Frederick became one of the founders of the black-owned Louisiana Life Insurance Company, known today as the Universal Life Insurance Company. Frederick filled the roles of a board member, secretary, vice-president, and president. Later, he became the principal stockholder. DeCuir discusses the importance of the black-owned insurance companies in softening the lines of division between the “American black and Creole economic elite.” Intermarriages among these board members and business alliances among the economic elites helped create prosperity and jobs for other blacks in the wider community (Decuir). Black physicians held very significant roles within their communities and the impact of their support for civil rights issues was potent in advancing the movement (Decuir). DeVore makes the point that Frederick maintained a degree of understatement in his public persona for several reasons related to desire to maintain influence and work diplomatically for his community:
… [He] allowed himself to be viewed only in non- controversial roles by the white community of New Orleans. He was seen as a humanitarian, a competent professional, and a champion of better medical care for blacks in Louisiana. With this special image, he was able to secure favors for many blacks from the white power structure.”67 Dr. Frederick played an instrumental role in the formation of the local NAACP Branch and remained a life member. He was also active in the Urban League and devoted time and gave money to solve problems within the black community.
(DeVore)
In 1913, Frederick departed from Sarah Goodrich Hospital to become a surgeon for the Southern Pacific Railway in New Orleans. He remained with the railroad until 1932 when he took up the position of Chief of Surgery at the Flint-Goodridge Hospital at Dillard University. Frederick stayed at Flint-Goodridge until 1950 as he built the Department of Surgery and trained many new surgeons. The expansive Frederick evolved and broadened his post-graduate teaching program by reaching out to collaborate with a diverse and integrated faculty from Tulane and Louisiana State University. Frederick’s biographer, Cherrie, memorialized this innovative surgeon’s achievement and leadership in the midst of intractable bias in some quarters of the profession:
Flint-Goodridge maintained its AHA standards and he enlisted the city’s finest white physicians to practice there along with its black physicians. He would continue to serve on the staff of Flint for more than forty years. In spite of all his accomplishments, Dr. Frederick was denied membership in both the American College of Surgeons and the International College of Surgeons for many years because of racism. (Cherrie)
In 1934, Frederick became the first vice-president of the National Medical Association. In 1935, he served as the New Orleans General Local Chairman for National Medical Association and was part of the committee to consider the establishment of the organization’s home (Amistad Research Center website, Historical Note).
Frederick married his second wife, Eloise Clarke and in 1939, his son Rivers Jr. was born.
In 1950, Frederick retired as Chief of Surgery at the Flint-Goodridge Hospital in 1950, and he became a Consultant in Surgery. In an article, “Dr. Rivers Frederick Receives Distinguished Service Award for 1951,” published by JNMA (1951), Dr. Frederick’s many awards and honors, reflecting his great achievements across a career of service, including the decades at Flint-Goodridge, were summarized:
He is a fellow of the International College of Surgeons and a diplomate of the International Board of Surgery. He is a member of the Louisiana and Orleans Parish Medical Societies and chief consultant of the Robinson Infirmary and Clinic. At the Annual Assembly of the International College of Surgeons in Florence, Italy in 1951, he was made a member of the Societa Tosco Umbra di Italia.
He has been an active community service as a member of the Medical Advisory Board of Flint-Goodridge Hospital of Dillard University, the New Orleans Executive Committee of the American Cancer Society, the Executive Committee of the New Orleans Tuberculosis Association, the Mayor’s Advisory Committee, the New Orleans Committee on Race Relations, and the Advisory Council to the Governor (Louisiana) on Civil Defense. He is an associate Medical Adviser to the Selective Service Board.
Dr. Frederick has been a recipient of numerous citations and honors. These include an Award of Merit for Outstanding Service, by the American Cancer Society, a Certificate of Recognition for Outstanding Achievement, by the National Urban League, a “Real Salute” from Radio Station WTPS (Music of New Orleans) in 1949, and honorary presidency of the New Orleans Urban League. In 1947 Dr. Frederick was honored at a public testimonial at Flint-Goodridge Hospital where a portrait was unveiled celebrating fifty years of medical practice.
…Dr. Frederick is a life member of the National Association for the Advancement of Colored People and a life member of the Louisiana Education Association. He belongs to the Chi Delta Mu and the Phi Beta Sigma fraternities. (Dr. Rivers Frederick Distinguished…)
Noting the absent mention of ACS in foregoing declaration, we note that the National Medical Association’s position at the time stands in stark contrast with that of the American College of Surgeons (ACS) in the same era. The discrimination of the ACS against black surgeons was very controversial in the 20th century. When the African-American surgeon, Dr. Thorne was rejected, no less than New York governor, Thomas Dewey launched an inquiry into the ACS’s blockade against their deserving fellow surgeons of color. According to Thomas Ward, author of Black Physicians in the Jim Crow South, the “firestorm” that called Dewey into action, also resulted in a sea change in the ACS, at least as it functioned in the North states:
…the ACS quickly amended its policy so that any certified surgeon was eligible for membership and stated that black physicians were not required to be members of the AMA if they lived in a region where they were excluded from their local AMA affiliate because of their race. Under this new policy fourteen black surgeons, all northerners, were soon elected to the fellowship.49 (Ward)
The story was different, however, in the South where the ACS local boards, like other specialties in the region, persisted in their discrimination toward black physicians. Ward tells the story of the moral war waged between the North-South surgical leadership in the late 1940’s. Remember, Frederick was known to both sides of the dispute Ward describes:
Rivers Frederick of New Orleans was a victim of this discrimination. The longtime chief of surgery at Flint-Goodridge Hospital, Frederick was denied membership to both the American College of Surgeons and the International College of Surgeon by local white physicians. In 1948, Ulysses Grant Dailey, chief surgeon of Chicago’s Provident Hospital and diplomate of the International College of Surgeons (ICS), protested the rejection of Frederick’s application to the society’s local director, William Bendel. Dr. Bendel informed Dailey that it was the wish of the New Orleans chapter of ICS not to admit Frederick to membership and that “we do not want you in Illinois trying to tell us in Louisiana what to do.” He added that “Dr. Fredericks [sic] application for membership has been rejected by the American College of Surgeons and I don’t know why you would want us to do different…[as] we feel that we have as good or a better organization.”50 (Ward)
Dr. Frederick died on September 2, 1954.
In her historical review and 2009 dissertation, “Attacking Jim Crow: black activism 1925-1941,” Sharlene Sinegal DeCuir offers this tribute to the extraordinary path cut by Rivers Frederick through the tumultuous days Jim Crow:
By the 1930’s, Frederick had become the most prominent black doctor in Louisiana and one of the best surgeons in the South. 59… The American black, Creole and white communities, viewed Frederick as a great doctor and true professional. He was a unifier in the American black and Creole communities. His insurance company, the Louisiana Industrial Life Insurance Company, employed both American blacks and Creoles. His family ties brought American blacks and Creoles together through business and private ventures. Frederick’s wealth and social status allowed him to provide financial support and secure favors for black organizations. He provided financial support for both the NAACP and the Urban League, but he preferred not to participate in forwarding their agendas because he did not want to undermine his favor with whites. He was one of the few Creole or American black doctors who worked with white patients. By the time of his death in 1954, Frederick’s assets totaled more than 1.5 million dollars. (Decuir)
How honored we have been by his presence among us and his service.
Works Cited
- Frederick, Rivers (1874-1956). Amistad Research Center, Tulane University, New Orleans, Louisiana. Biographical note on Rivers Frederick Papers. Accessed May 2020 at: http://amistadresearchcenter.tulane.edu/archon/index.php?p=collections/findingaid&id=18&q=&rootcontentid=6365#id6365
- Cherrie, Lolita V. “Overcoming Adversities: The Life of Dr. Rivers Frederick (1874-1954). On the CREOLEGEN website, March 16, 2013. Accessed May 2020 at: http://www.creolegen.org/2013/03/16/overcoming-adversities-the-life-of-dr-rivers-frederick-1874-1954/
- DeCuir, Sharlene Sinegal. “Attacking Jim Crow: black activism in New Orleans 1925-1941.” (2009), Accessed May 2020 at: https://digitalcommons.lsu.edu/gradschool_dissertations/1869
- DeVore, D. E. (1989). Race Relations and Community Development: The Education of Blacks in New Orleans, 1862-1960. Accessed May 2020 at:https://digitalcommons.lsu.edu/cgi/viewcontent.cgi?article=5838&context=gradschool_disstheses
- “Dr. Rivers Frederick Receives Distinguished Service Award for 1951.” Journal of the National Medical Association vol. 43,6 (1951): 400. Accessed May 2020 at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2617037/
- Ward, T. J. (2003). Black Physicians in the Jim Crow South. University of Arkansas Press.