Residency Curriculum
For more information, please email to resident coordinator at entresmanager@uic.edu.
Didactic Curriculum Heading link
July-September
Otology with Dr. Redleaf/Audiology with Dr. Matusik and her team
October-November
Laryngology with Dr. Sims
December-February
Rhinology with Drs. Joe and Lee
March-June
Head and Neck Surgical Oncology with Drs. Wenig and Lin
Monthly
Facial Plastics with Drs. Dayan, Dixon, Kerolus and Caughlin
Quarterly
Morbidity and Mortality lead by Dr. Lin
Quarterly
Journal Club lead by Dr. Weinreich
Quarterly
Research Lecture Series lead by Dr. Weinreich
Bi-monthly
PSQI Lecture Series lead by Drs. Weinreich and Rubenfeld
** All didactics include lectures by visiting professors
Clinical Rotations Heading link
-
Residency Rotations
Residency Rotations
Residency Rotations
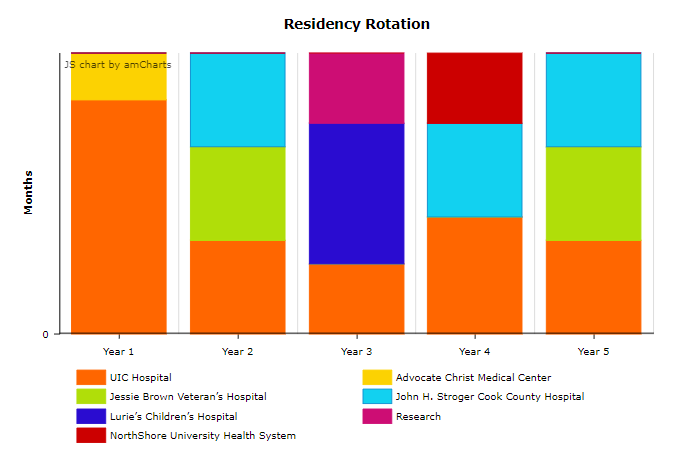
YEAR 1 UIC Hospital 24 weeks Otolaryngology-Head and Neck Surgery 4 weeks Anesthesia 4 weeks Plastic Surgery 4 weeks Radiology 4 weeks Emergency Medicine 4 weeks Vacation Advocate Christ Medical Center 4 weeks Surgical Intensive Care 4 weeks Trauma Surgery YEAR 2 4 months UIC Hospital 4 months Jessie Brown Veteran’s Hospital 4 months John H. Stroger Cook County Hospital YEAR 3 3 months UIC Hospital 6 months Lurie’s Children’s Hospital 3 months Research YEAR 4 5 months UIC Hospital 3 months NorthShore University Health System 4 months John H. Stroger Cook County Hospital YEAR 5 4 months UIC Hospital 4 months Jessie Brown Veteran’s Hospital 4 months John H. Stroger Cook County Hospital -
Curriculum Topics and Schedule
- What is Quality and Patient Safety?
- Care must be safe
- Care must be effective and reliable
- Care must be patient centered
- Care must be timely
- Care must be efficient
- Care must be equitable
- Quality improvement and pay-for-performance
- Introduction to Quality Improvement (Dr. Richard Banchs)
- Why?
- What are the basics?
- How to choose a QI project?
- What is the framework of a QI project?
- Why is this important at the resident physician level?
- What is the role of a sponsor?
- How to design and implement a QI project: the nuts and bolts (Dr. Ari Rubenfeld)
- PDSA cycle
- RCA
- Fishbone diagrams
- Pareto charts
- NSQIP (Dr. Ari Rubenfeld)
- How a big database works
- How to use the data
- Medical Legal aspects related to providing surgical care (Hospital Department Attorney)
- Risk Management (Rhonda Perna, Chief of Risk Management)
- Presentation from this department on who they are and the role they serve at UI Health
- Remove the stigma
- Review patient safety event reporting here and what the follow-up steps entail
- UI Health Culture of Safety & Current Initiatives (Jodie Joyce, Chief Quality Officer)
- UI Health culture of safety
- Current QI initiatives within our system
- Teamwork in the hospital setting (Shelly Major, CNO)
- Identify necessary elements to achieve teamwork
- Identify effective team leadership qualities
- Functional M&M (Dr. Ari Rubenfeld)
- Resident Presentations (Dr. Virginie Achim)
- What is Quality and Patient Safety?
List of Lectures – Otolaryngology Heading link
-
Basic Sciences
- Basic Perioperative Surgical Principles and Critical Care
- Reading and Understanding Medical Literature
- Genetics within Otolaryngology
- Microbiology, Otolaryngologic Infections, Antibiotic Therapy
- Surgical Pathologic Principles within Otolaryngologic Practice
- Neurology as it pertains to Otolaryngology
- Pain management
- Ophthalmology as it pertains to Otolaryngology
- Anesthesiology principles and Otolaryngologic Considerations, Managing the Difficult Airway, Intubation & Tracheotomy- Dr.Thambi
- Endocrinology as it pertains to Otolaryngology
- Geriatric Otolaryngology
- Systemic Autoimmune, Connective Tissue, Granulomatous Disorders of the Head and Neck
- Nasal, Oral, Laryngeal, and Tracheal Manifestations of Systemic Disease
-
FPRS
- Facial Analysis
- Digital Imaging and Traditional Photodocumentation
- Local Cutaneous Flaps and Grafts
- Tissue Expanders
- Scar Camouflage
- Nasal Reconstruction
- Facial Reanimation
- Surgical Anatomy of the Nose as it Pertains to Rhinoplasty
- Rhinoplasty: Analysis, Incisions and Approaches
- The Nasal Dorsum: Management of the Upper 2/3 of the Nose
- Nasal Tip Surgery
- Management of the Crooked Nose
- Revision Rhinoplasty
- Management of the Aging Forehead
- Upper Eyelid Blepharoplasty
- Lower Eyelid Blepharoplasty
- Rhytidectomy
- Management of the Aging Neck
- Otoplasty
- Chemical Peels
- Chin Augmentation
- Congenital Auricular Malformation and Managemetn
- Lasers in Facial Plastic Surgery
- Hair Restoration
- Cosmetic Uses of Neurotoxins and Injectable Fillers
- Management of Benign Facial Lesions, Keloids
- Wound Healing
-
General Otolaryngology
- Taste and Stomatitis
- Pharyngitis, Odontogenic Infections and Deep Space Neck Infections
- Head and Neck manifestations in the Immunocompromised host
- Evaluation and Management of TMJ Disorders
- Sleep Medicine for the Adult Patient and Medical Therapy
- Nasal, Palatal, Oropharyngeal, Hypopharyngeal, and Skeletal Surgery for OSAS
-
Head and Neck
- Molecular Biology of Head and neck cancer – HPV. Fundamentals of molecular biology and gene therapy
- Principles of Radiation Oncology in the head and Neck. Radiation Physics, Radiobiology and Clinical Principles
- Principles of Chemotherapy and Targeted Biologic Agents
- Cutaneous Malignancy, Non-melanoma
- Malignant Melanoma of the Head and Neck, Cutaneous and Mucosal Disease
- Salivary glands: Physiology, Inflammatory Disorders, Benign Neoplasms, Cancers, and Management
- Lip Cancer
- Neck Dissection
- Controversies in Management of the N0 Neck
- Differential Diagnosis of Neck Masses
- Oral Cavity: Physiology, Benign tumors, Cancer & Treatment
- Reconstructive Principles of the Oral Cavity
- Prosthetic Management of Head and Neck Defects
- Nasopharynx: Benign and Malignant Neoplasms
- Oropharyngeal Carcinoma, Surgical Approaches, Reconstruction
- Hypopharyngeal and Cervical Esophageal Carcinoma – Radiotherapy, Chemotherapy, and Reconstruction
- Early Laryngeal Cancer – Conservation Laryngeal Surgery – VPL, Supraglottic laryngectomy, SCL- CHEP/SCL-CHP
- Advanced Laryngeal Cancer. Reconstructive Principles of the Pharynx and Larynx
- Voice Rehabilitation following Laryngectomy
- Tracheal Tumors – Diagnosis and Management
- Lymphomas of the Head and Neck
- Orbital tumors
- Cranial Base Surgery
- Odontogenic Cysts and Tumors
- Treatment of Thyroid Neoplasms
- Hyperparathyroidism, Evaluation and Management (include management of Thyroid eye dz)
- Complications of Neck Surgery
- Minimally Invasive Head and Neck Surgery, including TOLS and TORS
- Management of Osteoradionecrosis- Reconstruction of the Mandible
- Reconstructive Principles of Microvasular Free Flaps
-
Laryngology
- Upper Digestive Tract Anatomy and Physiology
- Laryngeal and Pharyngeal Function- Assessment of Swallowing
- Esophageal Disorders and Diseases – Transnasal Esophagoscopy
- Management of Intractable Aspiration
- Glottic and Subglottic Stenosis: Evaluation and Management in the Adult
- Voice: Anatomy, Physiology, Clinical Evaluation and Therapy
- Laryngopharyngeal Reflux and Eosinophilic Esophagitis
- Infection, Infiltration and Benign Neoplasms of the Larynx
- Benign Vocal Cord Lesions and Phonomicrosurgery
- Evaluation and Treatment of Vocal Fold Paralysis (medialization thyroplasty, arytenoid adduction and abduction, laryngeal reeinnervation
- Neurologic Evaluation of the Larynx and Pharynx. Neurologic Disorders of the Larynx
- Care of the Professional Voice
- Office-based Laryngologic Procedures
-
Otology
- Anatomy and Physiology of Hearing
- Development of the Ear and Congenital Malformations
- Congenital Hearing Loss. Genetics of Ear Disorders and Sensorineural Hearing Loss
- Infections and Benign/Malignant Disorders of the External Ear
- The Chronic Ear and Conductive Hearing Loss. Eustachian Tube Dysfunction
- Otosclerosis
- Otitis Media
- Chronic Otitis Media with Cholesteatoma
- Sensorineural Hearing loss. Hyperacusis. Treatment of Tinnitus
- Auditory Rehabilitation
- Acoustics and Lateral Skull Base
- Otologic Manifestations of Systemic Disease (Excluding Autoimmune inner ear disease)
- Facial Nerve. Anatomy, Tests of Facial Nerve Function, Infratemporal Facial Nerve Surgery
- Peripheral Vestibular Function Testing
- Peripheral and Central Vestibular Disorders. Surgery for Vestibular Disorders
- Autoimmune Inner Ear Disease
- Diagnostic Audiology
- Electrophysiologic Assessment of Hearing. Neurophysiology and ABR
- Cochlear Implantation: Patient and Device Selection. Outcomes, Rehabilitation, and Education
- Hearing Aid Amplification, ALD’s, Tinnitus
- Temporal Bone Neoplasms and Lateral Cranial Base Surgery
- Neoplasms of the Posterior Fossa
- Temporal Bone Histopathology
- Auditory Processing Disorders
-
Pediatric
- RRP
- Pediatric Head and Neck Malignancies
- Pediatric Neck Masses
-
QI
- Safety and Quality Assessment in Otolaryngology
- Compliant Documentation, Coding and Billing in the Practice of Otolaryngology
- Telemedecine for Otolaryngology
- Conflict of Interest
- Outcomes Research
- Interpreting Medical Data
- Evidence Based Performance Measurement
-
Radiology
- Temporal Bone
- Head and Neck
- Diagnositic Imaging of the Larynx
- Sinus Imaging
- Imaging of the Pharynx and Esophagus
- Ultrasound Imaging of the Neck
- Interventional Neuroradiology of the Skull Base, Head and Neck
-
Rhinology and Allergy
- Sinonasal Anatomy, Physiology and Olfaction
- Immunology, Allergy and Allergy Testing
- Diagnostic Tools for Sinonasal Disease. Objective Assessment of Nasal Function
- Management of Intractable Aspiration
- Epistaxis
- Acute Rhinosinusitis – Pathogenesis, Treatment, and Complications
- Fungal Rhinosinusitis
- Results of Medical and Surgical Treatment of Chronic Rhinosinusitis W and W/o Nasal Polyps
- External Approaches to Sinus Surgery for Chronic Rhinosinusitis
- Correction of Nasal Obstruction, Septoplasty, Inferior Turbinate Reduction
- Endoscopic orbital and lacrimal surgery. Dacryocystorhinostomy
- Complications of Sinus Surgery
- CSF Rhinorrhea: Endoscopic Evaluation and Treatment
- Frontal Sinus Surgery
- Neoplasms of the Nose and Paranasal Sinuses
-
Trauma
- Principles of Trauma, Management of Facial Soft Tissue Injury and Burns
- Penetrating Face and Neck Trauma, Laryngeal Trauma (penetrating and blunt neck and laryngeal trauma)
- Principles of Rigid Fixation of the Facial Skeleton and Surgical Approaches
- Mandibular Fractures
- Midfacial, Orbital & Nasal Fractures
- Frontal Sinus Fractures
- Fracture Management within Pediatrics
- Management of Temporal Bone Trauma
Hands-On Courses Heading link
- Sinus Dissection
- Temporal Bone Lab
- Soft Tissue Dissection
- Rhinoplasty/ Face Lift
- Injectables