Understanding Deep Brain Stimulation (DBS) for Parkinson’s Disease
Understanding Deep Brain Stimulation (DBS) for Parkinson’s Disease Heading link

April is Parkinson’s Disease Awareness Month, an opportunity to recognize those battling the stifling disease and to bring awareness to the many medical advances offered by UI Health.
Parkinson’s disease (PD) is the second-most prevalent neurodegenerative condition in the U.S. While most cases are diagnosed in individuals over 60, some under 50 are prone to the disease. Roughly 500,000 Americans live with PD, though many remain undiagnosed or misdiagnosed, suggesting much higher cases.
UI Health offers the innovative treatment of Deep Brain Stimulation (DBS) for Parkinson’s disease, a targeted, non-invasive procedure that uses electrical impulses to restore brain function. This groundbreaking therapy marks a turning point in managing Parkinson’s symptoms, providing patients with a personalized, long-term solution for improved quality of life.
What is Parkinson’s disease? Heading link
PD is a progressive disorder triggered by degeneration of nerve cells in the part of the brain that directs movement. These nerve cells either become severely impaired or decay, causing the loss of dopamine, an essential chemical transmitter.
As a neurotransmitter, dopamine directs parts of the brain through cognition and bodily functions to seek motivation, learning, and gratification. Akin to a GPS system, dopamine aids in navigating decisions by signaling where to go. In PD, this GPS begins to fail, misfiring these signals, leading to deviations, delays, slowness, and halts. Without clear direction, the brain struggles to coordinate even the most basic motor tasks.
Common motor symptoms of PD include misperception, tremors, muscle rigidity, involuntary movements, and difficulty walking and balancing. These symptoms often worsen over time and significantly impact daily activities. Non-motor symptoms are also common, including cognitive impairment, mental health disorders, and sleep and sensory disturbances. As the disease progresses, many individuals may develop dementia.
While the exact cause of PD remains unknown, it is believed to involve genetic and environmental factors. Certain genetic variations have been shown to increase a person’s risk, though how these genes contribute to the disease is still not fully understood. Some research has shown that pesticides and pollution may play a role in the development of PD.
Deep Brain Stimulation (DBS) Heading link
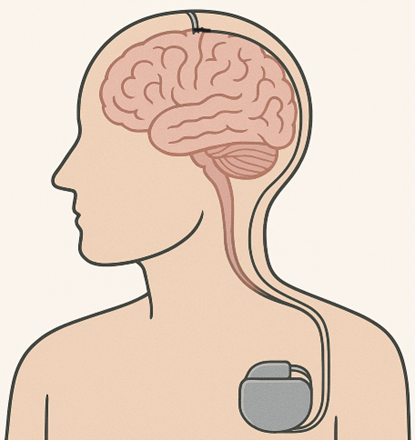
Just as a pacemaker regulates abnormal heart rhythms by sending electrical signals, DBS utilizes a pacemaker-like device to deliver controlled electrical impulses to specific brain areas to correct abnormal neural activity.
DBS targets the misfiring of information, interrupting the electrical signals that cause these debilitating symptoms and helping restore normal movement and function. The precise placement of the electrodes is crucial, so advanced imaging, neuropsychological tests, movement assessments, and brain mapping are used to ensure accuracy while avoiding healthy tissue.
To ensure the DBS electrode is placed in the right spot in the brain, doctors use a technique called microelectrode recording (MER). This involves guiding a small wire into the brain to listen to the activity of individual brain cells. By doing this, they can confirm when they’ve reached the correct area and map out its size, helping them place the DBS electrode as precisely as possible. This ensures that part of the electrode stays above the target, effectively stimulating the entire region.
“Every part of the brain has its own function,” said Dr. Konstantin Slavin, a neurosurgeon and professor at the University of Illinois Chicago (UIC). “That’s why finding the exact spot to place the electrode is important to avoid unwanted side effects.”
Real-time report Heading link

The procedure itself begins with minor holes drilled into the cranium to insert the electrodes into the targeted brain area. “It’s a small drilling but crucial. Our anesthesiologist is there to ensure the patient feels no discomfort,” said Dr. Slavin.
The neurosurgeon then implants a thin wire, called a lead, into the brain region. After the electrodes are positioned, the neurostimulator device is implanted beneath the skin near the collarbone. This device is connected to the electrodes and delivers controlled electrical signals to specific areas of the brain. These pulses help stabilize abnormal brain activity, easing symptoms.
While anesthesiologists are there to administer medicine to patients who wish to be asleep during the procedure, surgeons often prefer patients to be conscious with pain medication. “We really want patients to be awake and functional to see how their symptoms respond. We heavily rely on patients’ real-time reports to manage their symptoms and fine-tune electrode placement,” Dr. Slavin explained. Patient feedback helps mitigate side effects and intensify accurate treatment.
“Every part of the brain has its own function,” Dr. Slavin said. “If the patient’s electrodes are too close to the sensory part of the brain, they can feel a tingle or abnormal movements when the device’s battery is turned on. However, these can be modified by adjusting the electrodes’ perimeters.”
The neurostimulator device is rechargeable and can last up to 15 years with proper maintenance. Patients use a wireless charger placed over the collarbone skin over the implant site. This charger communicates with the battery beneath the skin, transmitting energy safely and effectively to keep the system powered. Regular charging becomes a part of the routine, helping ensure consistent symptom relief.
“When they do well, then we expect to hear from patients every six months,” said Dr. Slavin. “If they require any adjustments, we can see them however often they’d like to fine-tune the treatment.”
The results are in Heading link
During Parkinson’s Awareness Month, it’s crucial to highlight the exceptional impact of DBS in managing PD.
Although not a cure, DBS offers meaningful relief from the challenging motor symptoms of Parkinson’s disease, giving many patients the chance to reclaim parts of their daily lives. Unlike medications that can diminish effectiveness over time, DBS delivers long-term benefits—reducing involuntary movements and mitigating cognitive disruptions—helping patients regain control and improve their overall quality of life.
“We are very focused on the individualization of treatment,” said Dr. Slavin. “We approach each patient individually and make decisions based on imaging, family history, personal preferences, and beliefs. We offer various interventions and guide patients based on what feels right for them.” This personalized, team-based approach—drawing on the expertise of neurologists, neurosurgeons, psychologists, radiologists, and physical therapists, establishes DBS as a transformative procedure.